Don Ruch’s family thought round-the-clock care would help him recuperate, but he ended up in intensive care in septic shock, suffering from “severe” malnutrition, bedsores on his pelvis and back, a burn on his right thigh and a trauma wound. USA TODAY
World War II veteran Rosario "Russ"
Bonanno was facing worsening dementia when his family brought him last
year to the Department of Veterans Affairs nursing home in Bedford,
Massachusetts. He had been in assisted living, but after six years, some
family members thought he needed more specialized care.
Within
days after Bonanno arrived, his son Nick said the 93-year-old was
“dazed, confused, disheveled" as staff began medicating him. He wasn’t
the only resident who looked drugged. "Everyone looks like a zombie,"
Nick said.
What Nick and his family didn’t know was
that the Bedford facility ranked among the worst of 133 VA nursing
homes across the country, in part for giving so many residents
anti-psychotic drugs.
But the VA knew.
The
agency has tracked detailed quality statistics on its nursing homes for
years but has kept them from public view, depriving veterans of
potentially crucial health care information. Nearly half of VA nursing
homes nationwide – 60 – received the agency'slowest ranking of one out of five stars as of Dec. 31, 2017, according to documents obtained by USA TODAY and The Boston Globe.
The VA made some of its ratings public last week after
receiving questions from the Globe and USA TODAY about all the secrecy.
VA officials said President Donald Trump wanted to release the ratings
all along and blamed the Obama administration for not making them public
earlier.
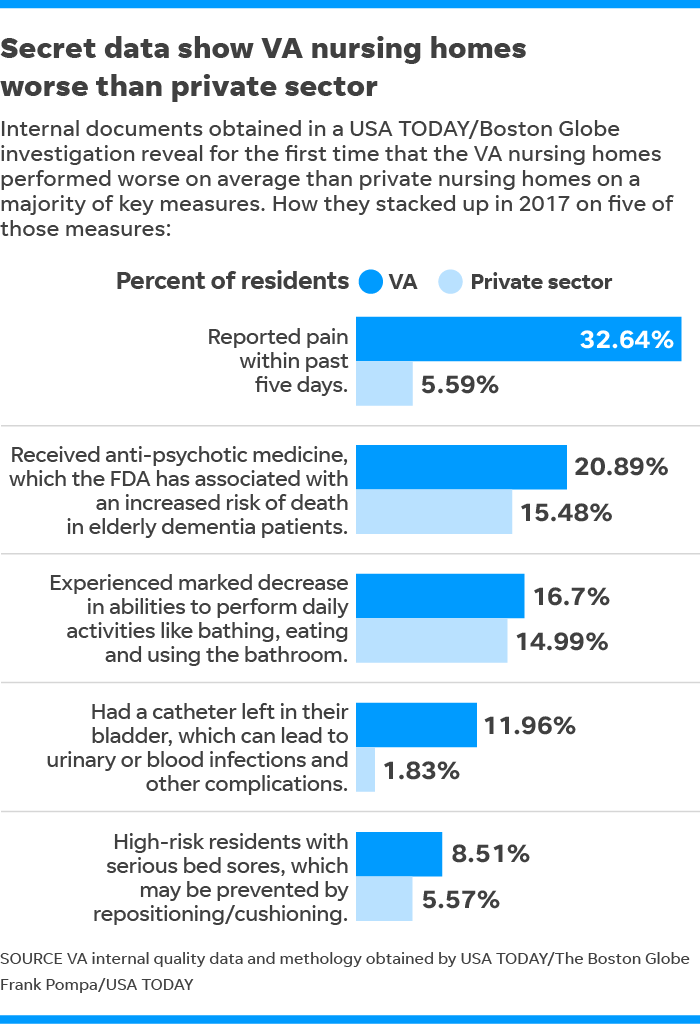
Statistics the VA has not released paint a
picture of government nursing homes that scored worse on average than
their private sector counterparts on nine of 11 key indicators last
year, including rates of anti-psychotic drug prescription and residents’
deterioration. In some cases, the internal documents show, the VAratings
were only slightly worse. In others, such as the number of residents
who are in pain, the VA nursing homes scored dramatically worse.
The
worst-performing VA nursing homes were scattered across 32 states,
including Pennsylvania, which had five one-star facilities, as well as
Texas and California, which had four each. The VA facility in Bedford
and another in Brockton, Massachusetts, were the only one-star nursing
homes in New England.
VA
officials argued that the VA nursing home system, overall, “compares
closely” with private nursing homes despite caring for typically sicker
residents.
VA spokesman Curt Cashour called it
“highly misleading” to compare pain levels at the VA with those at
private nursing homes because VA residents have “more challenging”
medical conditions. The VA's internal quality tracking found that VA
nursing home residents were five times more likely to report being in
pain than private nursing home residents.
Cashour
said 60 VA nursing homes have seen improvements in their rating over the
past year, while only one had a “meaningful” decline.
“We
are committed to continuous improvement efforts in all of the (VA
nursing homes) and demonstrating performance that is as good (as) or
better than private sector facilities,” Cashour said.
The
VA’s hospitals have drawn intense criticism for repeated scandals
involving health care in recent years, including preventable deaths, but
the agency largely has operated its nursing homes with scant public
scrutiny. VA nursing homes serve 46,000 veterans annually in 46 states,
the District of Columbia and Puerto Rico.
Internally,
the agency has long monitored care at its nursing facilities through
quality indicators and unannounced inspections and, since 2016, through
star rankings based on the indicators. Until now, it has kept all of
these quality measures from the public.
Under
federal regulations, private nursing homes are required to disclose
voluminous data on the care they provide. The federal government uses
the data to calculate quality measures and posts them on a federal
website, along with inspection results and staffing information. The
regulations do not apply to the VA.
The
VA has “got this whole sort of parallel world out there that’s hidden,”
said Robyn Grant, director of public policy and advocacy at the
National Consumer Voice for Quality Long-Term Care. “I still can’t get
over that this information is not available to people who are looking
for a veteran’s home. That’s just unacceptable.”
VA
spokesman Cashour blamed the Obama administration for resisting making
quality data public. “But under President Trump’s leadership,” he wrote
in a statement June 12, “transparency and accountability have become
hallmarks of VA.”
The VA’s decision to release the
quality data came after first asking USA TODAY and the Globe for more
time to answer questions about the secret ratings. Then the VA released
the quality ratings while the reporters waited for answers.
The agency did not release the more detailed information that underlies the star ratings, such as rates of infection and injury.
Alex
Howard, a longtime transparency advocate and former deputy director of
the Sunlight Foundation, said the VA should release all of the data
immediately – and on an ongoing basis. He said the underlying
information is critical to understanding what the stars mean.
“There
shouldn’t be a gap between the reality of how we’re treating people
under the government’s care and public understanding of it,” Howard
said. “This is not a situation where we’re concerned about some matter
of national security, this is simply being honest about how well things
are going.”
'I was told how good it is – by VA, of course'
After 38 years of marriage, Leslie Roe made the gut-wrenching decision to place her husband in a nursing home.
Earl
James “Jim” Zook, 72, suffered from dementia and had taken to wandering
away from their home in Coosada, Alabama, and she worried she would
lose track of him.
Roe moved Zook, a Vietnam-era
Navy veteran, into a VA home an hour away in a rural, wooded swath of
Tuskegee, Alabama. She said VA staff put a bracelet on his wrist warning
he was a flight risk and placed him in a secure ward.
Three
months after Roe checked Zook into the Tuskegee facility, staff lost
track of him. Zook simply walked out into the woods; Roe said she was
told there was a faulty door.
She had no idea that
the facility ranked among the worst VA nursing homes in the country last
year, scoring only one out of five stars in the agency’s own quality
rankings. She had to rely on what the VA said.
“I was told how good it is – by VA, of course,” Roe said.
The
VA assigns stars based on 11 indicators that can be tipoffs to larger
problems with overall quality. For example, high rates of falls or bed
sores may indicate understaffing or neglect.
The
Tuskegee nursing home scored worse than private nursing home averages on
eight of the 11 criteria as of Dec. 31, 2017, including rates of
residents being in pain, receiving anti-psychotic drugs and contracting
urinary infections.
This year, the Tuskegee nursing home improved from one star to two stars. That was too late for Zook.
He
hasn’t been seen since he walked out of the Tuskegee facility in
January 2017. Searches by helicopter and with tracking dogs turned up
nothing.
“We finally declared him legally dead,”
Roe said this year, “because there was no way he could have lived
without his medication.
“Anybody that deals with VA, I feel sorry for them,” she said.
Cashour
said that after Zook’s disappearance, which he called an “unanticipated
outcome,” the VA implemented more safety measures, including adding GPS
to an alarm system that notifies staff if patients leave the facility.
‘They break their spirit’
The
VA has relied for more than a decade on an outside company,
Wisconsin-based Long Term Care Institute, to conduct inspections of VA
nursing homes and report back to the agency.
The VA
banned the public release of institute reports after the Pittsburgh
Tribune-Review in 2009 published the findings from one report detailing
“significant issues” at the VA nursing home in Philadelphia, including
poor resident grooming and pest control. In one case, a patient’s leg
had to be amputated after an infection in his foot went untreated for so
long his toes turned black and attracted maggots.
The
VA said the reports are internal quality assurance documents
“protected” from disclosure under federal law. However, in their
announcement last Tuesday releasing the nursing homes’ star ratings, VA
officials said they would also release the long-term care reports. They
didn’t say when.
Such reports might have been
helpful to Bonanno, the WWII veteran whose family moved him from a
private assisted-living facility to the Bedford VA last April as his
dementia worsened.
An
inspection report obtained by the Globe shows reviewers from the Long
Term Care Institute found several instances of neglect at the nursing
home in April 2017. They saw a veteran lying in bed covered only by a
urine-and-feces-stained sheet. They saw another veteran struggling to
eat, using his hands to shove food in his mouth after trying
unsuccessfully to maneuver food onto a spoon. Staffers were nearby, the
report said.
By then, inattentive patient care in
Bedford had already proved fatal to one resident. Vietnam veteran Bill
Nutter died in 2016 while an aide who was supposed to check on him
hourly allegedly played video games on
her computer and didn’t check on
him at all. She later resigned, and Nutter’s family sent a letter to the
VA seeking $10 million in damages.
Bonanno’s family would learn about the conditions the hard way.
His
son said Bonanno, a happy-go-lucky retired mechanic, would always wake
up early for breakfast. But for the first few months in the Bedford
facility, he was fast asleep when his son arrived after 11 a.m. for a
visit. According to Nick, the staff woke him up at 6 a.m. to put him
back to sleep. They gave him an anti-psychotic drug and a sedative, Nick
said.
“They medicate them until they break their
spirit and make them passive. I guess it’s easier for the staff to deal
with them,” Nick said. “In six years in assisted living, he’d never been
medicated during the day.”
Staff told Nick that his father was “agitated” and needed the medication — a contention Nick disputes.
Cashour
said many of the veterans at Bedford live with “chronic mental illness”
related to their military service and require psychotropic medication
“to reduce distress and manage behavior.” After the veteran is
stabilized, he said, the VA works to reduce the use of these drugs.
Nick’s
brother, Russ, who lives in Indiana, said he and his sister, who also
lives outside of Massachusetts, believe their father’s overall health
has improved and he is properly medicated.
“My sister and I both agree he’s getting care that’s high quality and appropriate for his needs,” he said.
Nick
said that as their father became more and more groggy, he participated
in fewer activities; he went from walking with help to sitting in a
chair for hours, doing nothing.
“There are ways to
care for people with dignity and allow them to be themselves,” said
Nick, who visits his father several times a week. “I was lucky to have
Dad in a place that was pretty good for six years. It was a huge
drop-off in the way they provide care at the VA versus a private
facility.”
‘I thought my heart was going to stop’
Even
higher-ranking VA nursing homes scored below private nursing homes on
individual quality measures last year, the internal documents show.
The VA assigned three stars to its nursing home in Livermore, California, even though the facility scored
worse on average than private facilities on six of 11 criteria.
Residents reported being in pain at dramatically higher rates and
experienced general declines and developed sores at slightly higher
rates.
As a paraplegic, Livermore VA resident Don
Ruch couldn’t feel the gaping wound festering on his leg. When the
71-year-old saw a picture of the hole, he went from trusting to
terrified.
His family had moved him into the VA
nursing home last year, hoping the round-the-clock care and
rehabilitation services would help him recuperate from the aneurysm that
caused his paralysis.
Within months, the onetime
Army infantry radio operator ended up in the intensive care unit at a
nearby private hospital, Stanford ValleyCare. Doctors found him in
septic shock from a “significant” urinary tract infection, medical
records show. He was suffering from “severe” malnutrition, bedsores on
his pelvis and back, a burn on his right thigh and a trauma wound on the
back of his right calf.
Ruch couldn’t lift his leg to see the wound, so he asked a caregiver to take a picture and show it to him.
“I saw a hole in my leg that I think I can stick a golf ball into,” he said. “I thought my heart was going to stop.”
Ruch,
who said he was so depressed he didn’t realize he wasn’t eating enough,
felt betrayed — by the nurses who had repeatedly changed his bandages
without saying anything about how bad the wound had become and by the
doctor who told his family it was nothing to worry about and from a
“small bruise.” The same doctor told his niece he was malnourished
because “we can’t make a veteran eat.”
Don Ruch served as Army infantry radio operator in Vietnam from August 1968 - May 1970.
(Photo: Handout)
Cashour,
the VA spokesman, said Ruch has a complex medical history and a review
of his medical records “does not suggest that there was a delay in
diagnosis, treatment or triage to the hospital in this case.”
The
episode triggered Ruch’s post-traumatic stress disorder and his niece
managed to get him transferred to a private nursing home — paid for by
the VA — near her home in Omaha, Nebraska. It took three months to
recover, but he’s better, his family said.
Full Article & Source:
Secret VA nursing home ratings hide poor quality care from the public

No comments:
Post a Comment