Surveillance video captured the deadly blow to the head of 91-year-old
James “Milt” Ferguson Sr. Specialists say it could have been prevented.
USA TODAY
Jim Ferguson wanted answers.
Jim Ferguson wanted answers.
How
was his 91-year-old father, who served in the U.S. Navy in World War
II, fatally injuredin a Veterans Affairs nursing home, the institution
Ferguson had entrusted to care for him?
Huddled
around a computer monitor with managers at the VA in Des Moines, Iowa,
Ferguson watched a hallway surveillance video that depicted a chilling
blow to his father's head.
“I lost it,” Ferguson told USA TODAY. “I broke down.”
In
the video, James “Milt” Ferguson Sr., who had dementia and was legally
blind, appears confused. He opens a hallway door, rolls his wheelchair
into another resident’s room, then wheels back out. No staff members are
visible. He circles around and heads back into the room.
Halfway through the door, his chair flips over backwards. Milt Ferguson crashes
to the floor, landing on the back of his head. Ferguson said he was
told the chair was pushed over by the resident in the room, who can't be
seen in the video. As staff members rush to assist him, Ferguson is
able to turn over and sit up, but the impact causes a massive brain
bleed that will kill him within days.
What later
would turn the son’s despair into outrage was what he learned about
events leading up to his father wheeling around unsupervised last
December, and what happened after he smashed into the floor.
“It’s like my dad died at their hands,” Ferguson said.
Serious problems with resident care have occurred in many VA nursing homes across the nation, including the one where Ferguson was being cared for.
USA TODAY reported in March that inspections by a private contractor hired by the VA found deficiencies that caused "actual harm" to veterans at
more than half of the 99 VA nursing homes reviewed. The inspections
found inadequate supervision or hazardous conditions at 53 of them.
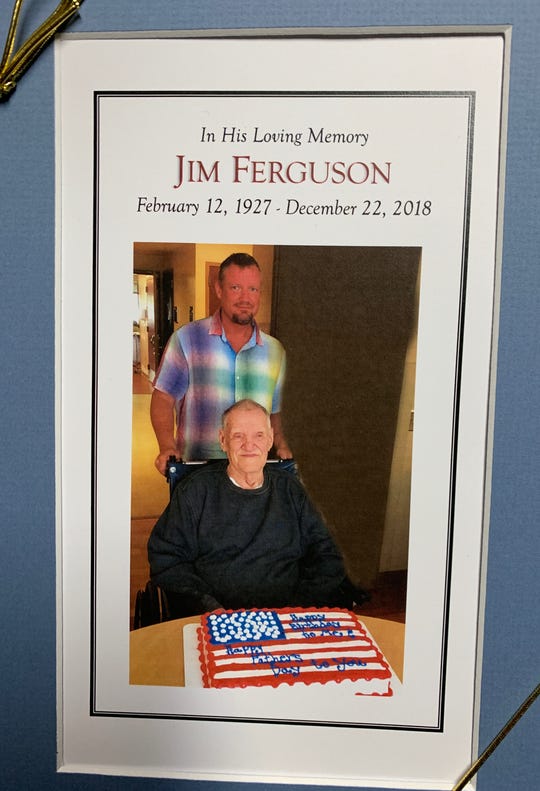 |
| James “Milt” Ferguson Sr. remembrance. (Photo: Family Photo) |
The story of what happened to James Ferguson in Des Moines provides a deeper picture of the care one elderly veteran received. Medical records provided to USA TODAY by his son and legal guardian outline what specialists say was a concerning series of decisions by VA staff, before and after his deadly head injury.
Nine
days before, VA caregivers determined Ferguson was a danger to himself
and others because his dementia caused him to wander around, agitated.
They had him on continuous one-on-one observation with an aide, but took
him off the strict monitoring when he entered the VA nursing home.
There, staff didn't reinstate the heightened observation, despite his
repeatedly straying dangerously into other residents' rooms.
After
his injury, staff put him back in his wheelchair but did not report the
incident to a supervisor for 40 minutes, the records and surveillance
video indicate. Ferguson wasn't transported to an emergency room for two
hours after that. Then, it took 2½ hours more to send him to a trauma
hospital. The time stamp on the video showed the fall occurred at
3:49 p.m. and it wasn't until just before 9 p.m. that Ferguson was
transported to the trauma facility.
'A disaster waiting to happen'
Specialists who reviewed Ferguson's medical records at the request of USA TODAY expressed concern about the quality of his care.
"It
was definitely a disaster waiting to happen, and it did," said Robyn
Grant, director of public policy and advocacy at The National Consumer
Voice for Quality Long-Term Care, a Washington-based nonprofit advocacy
organization.
"I just am really struck by the
predictability with his repeated episodes of going into other people's
rooms," she said. "They should have had some intervention so they could
provide him with adequate supervision and address the wandering."
Grant
said the length of time it took afterward to adequately evaluate and
diagnose the severity of his injury and get him to a trauma
facility also raises questions. "What was happening there, in terms of
those delays?" she said.
Richard Mollot, executive director since 2005 of the
Long Term Care Community Coalition, a New York City-based nonprofit
advocate of nursing home care improvement, said the shortfalls indicate
there was "very likely" a lack of skilled or adequately trained staff to
meet his needs.
"The point of being in that environment is that you have skilled nursing care and monitoring," he said.
Mollot
said the reporting delay is particularly concerning. "How often does
this happen that no one's looking at? That's what is so upsetting."
'All staff acted properly'
A
spokesman for the Des Moines VA, Timothy Hippen, said in a statement
that a review after the "untimely death" concluded "all staff acted
properly."
"Any time an unexpected death occurs, VA
Central Iowa Health Care System reviews its policies and procedures to
see if changes are warranted," he said. "We did that here, finding that
all staff acted properly."

In response to questions about the case, national VA spokesman Curt Cashour accused USA TODAY of focusing on "isolated complaints" and "cherry-picking the experiences of a handful of veterans to create the impression of a broad problem."
Cashour maintained
that, overall, VA nursing homes "compare closely" with non-VA
facilities. More than 40,000 veterans rely on care at the agency’s 134
nursing facilities each year.
USA TODAY reported last year that about 70% of VA nursing homes scored worse than non-VA nursing homes on a majority of quality indicators tracked by the agency, which include rates of infection, serious pain and bed sores.
Hippen declined to respond to detailed questions about Ferguson's case.
"We
will not be addressing the specifics of this case publicly, but we have
been in direct contact with the veteran’s family to discuss their
concerns," he said.
Jim Ferguson said he remains
upset even though VA officials shared the surveillance video with him
and said they were sorry about what happened to his father.
He wants VA staff held accountable. He wants to make sure policies are in place so it doesn't happen to anyone else.
“No
one should live their life like that and have what happened to him in
the end,” he said. “I want this to be the last person this happens
to.”
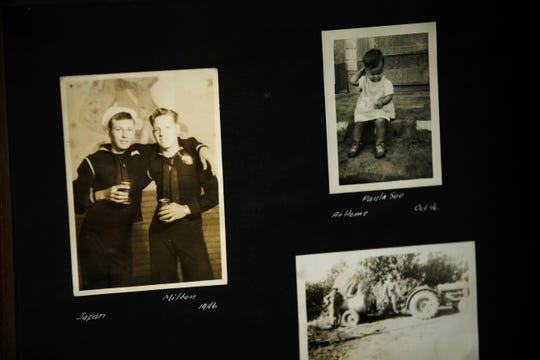
A gambler called ‘booger’
Even as his dementia worsened, Milt Ferguson flashed glimmers of his younger self.
The former deckhand on the heavy cruiserU.S.S.
Pensacola was affectionately known as “booger” at the Des Moines
Register, where he worked bundling newspapers for 23 years before
retiring in 1995. He loved to play the slots and the horses.
On
a note in his medical record, a nurse practitioner wrote: “Patient
laughs when his nickname is mentioned.” Jim Ferguson had come for a
visit that day, as he did most days. “He was smiling and appeared to be
enjoying his son’s company,” the medical record said.
The
decision to place him in a nursing home had been a gut-wrenching one,
Ferguson said. He had moved in with his parents and cared for them for
three years. But in April 2018 his mother died. He said a VA social
worker told him his father needed more intensive, round-the-clock care
and supervision.
“They made it sound like, well, if
he got hurt, I could be charged with a crime,” Ferguson said. “So
that’s when I decided to place him in a nursing home.”
‘His dementia was acting up’
Ferguson
moved his father to Bishop Drumm Retirement Center, a private facility
just outside Des Moines, where his mother worked as a nursing assistant
in the Alzheimer’s unit for more than 20 years before retiring.
The center took in Milt Ferguson last August. But three months later, his condition worsened.
"The day before Thanksgiving, I got a call from Bishop Drumm – his dementia was acting up," his son said.

He
hit two staff members, was “agitated all day” and was “wandering into
other residents room(s), causing distress,” a nurse later noted in
his medical record. “He is generally ‘sweet’ so this is a departure from
his usual behavior.”
Ferguson was taken by
ambulance to the Des Moines VA Medical Center, where he was admitted to
the acute psychiatry ward. He was put on one-on-one observation with a
sitter – an aide tasked with intervening if he lashed out or tried to
stray into other patients’ rooms.
They adjusted his
medications, and, after a few aggressive outbursts, he appeared calm
enough after three weeks to transfer into the VA nursing home on the
medical center’s campus.
But there was a catch, a psychiatric nurse wrote in his record: "Veterans are not put on sitter status over there."
‘Help me, help me’
After a 22-hour trial period without a sitter, Milt Ferguson moved in to the VA nursing home.
Problems began within hours.
He
hardly slept, he hallucinated, he called out "help me, help me" over
and over again. He was agitated and again, he "wandered into and out of
peers rooms" day after day, nursing staff wrote in his record.
They gave him medication. Sometimes he calmed down. Sometimes he didn’t.
A
psychiatrist was managing his case remotely. According to public
records, the doctor worked at a VA facility a few hours away in Lincoln,
Nebraska. Through virtual appointments, the psychiatrist advised
changes to Ferguson's medication.
On December 19, a
week after Ferguson moved in, nursing home staff noted he was still
restless and anxious, pacing and screaming and yelling. His care team –
psychiatrist, primary care doctor, nursing staff and social workers –
met to discuss the case.
The psychiatrist said a
review of his records showed "increased confusion with wandering" during
the past week. The doctor prescribed higher dosages of a
mood-stabilizing drug and a sedative. There was no discussion of closer
supervision or reinstatement of one-on-one observation, the records
show.
“Will ask RN to contact this MD in one week with update,” the psychiatrist wrote.
By then, Ferguson would be dead.
‘A golf ball-sized lump’
On
December 20, when two aides rushed to help Milt Ferguson, his head on
the floor and legs crumpled to the side, the time stamp on the hallway
surveillance video reads 3:49 p.m. But in a report filled out an hour
later, a nurse recorded the time of the accident as 4:30 p.m.
His
records do not indicate what the staff did with Ferguson during the
41 minutes in between, aside from putting him back in his wheelchair.
By
that time, he had a “golf ball-sized lump on the back of his head.” The
nurse notified the manager on duty, a nurse practitioner, who wrote at
5:06 p.m. that he had ordered an immediate CT scan of his head.
That
didn’t happen until about 6:30 p.m., when Ferguson arrived in the
emergency department of the medical center on the Des Moines VA campus,
on a bed wheeled by a nursing home aide. The aide said Ferguson had
earlier been taken for a CT scan but was uncooperative.
An
emergency room doctor quickly had a sedative administered and the scan
was completed. By that point, the World War II veteran had a “large
bleed” in the back right side of his brain that was so acute, the CT
report says his brain had shifted to the left inside his skull.
Sent 'to scanning’
The
doctor notified MercyOne Des Moines Medical Center, a trauma hospital,
at 7 p.m. For nearly two hours, the doctor tried to keep Ferguson
comfortable and his blood pressure under control until an ambulance
arrived and took Ferguson to Mercy at 8:55 p.m.
The doctor also kept calling Ferguson’s son, leaving voicemails.

But
Jim Ferguson had himself been admitted to a hospital and had provided
the VA nursing home with a consent form authorizing staff to contact a
close friend if anything happened to his father. That form had been sent
"to scanning” that morning.
When Jim Ferguson retrieved all the voicemails, he rushed to Mercy the next morning.
"He
was not responsive. He was laying on his bed, making this horrible
noise as they sucked saliva out of his mouth," he said. "I never even
got to say any last words to my dad."
He died the next day.
Specialists
who reviewed the case at the request of USA TODAY singled out multiple
shortfalls in his care at the VA that may have affected the outcome.
Grant,
the policy director at The National Consumer Voice for Quality
Long-Term Care, said the 22-hour trial of having no sitter was "not
enough time to establish how he was doing."
When
he then acted out day after day, in agitation and confusion, they
should not have allowed him to wander into other residents' rooms, she
said. Such situations can cause the other residents to lash out in fear
or distress and "lead to an altercation or violence or striking out."
"One
would argue that could have been prevented," she said. "There should
have been somebody, somewhere who could have seen that this happened and
– particularly when he wheeled himself – to have gone in and
intervened, 'Let me help you, let's go to your room.'"
Mollot,
the executive director at the Long Term Care Community Coalition, said
meeting the standards of care means staff identifies risks and needs and
ways to meet them and mitigate them and then does so consistently.
"This is exactly the kind of thing that happens when those standards are not followed," he said.
'A safe place'
The
spokesman for the Des Moines VA, while declining to answer detailed
questions about what happened, said that in general, "caring for nursing
home residents involves balancing patients’ independence with the need
for supervision, as appropriate."
"While tight
scrutiny and strict limits on residents’ activities and freedom of
movement could possibly lower the risk for adverse events, it would also
severely degrade patients’ quality of life, which is precisely what we
are trying to preserve for as long as possible," he said.
Jim
Ferguson still has his father’s wheelchair in the garage. He keeps the
sweatshirt his father was wearing when he last used the chair.Ferguson has retained a lawyer, Brad Biren, to help him figure out next steps and how to hold the VA accountable.
“Somebody didn’t watch my dad and let him die,” he said. “It’s supposed to be a safe place.”
Full Article & Source:
‘My dad died at their hands’: WWII vet fatally injured in VA nursing home

No comments:
Post a Comment