|
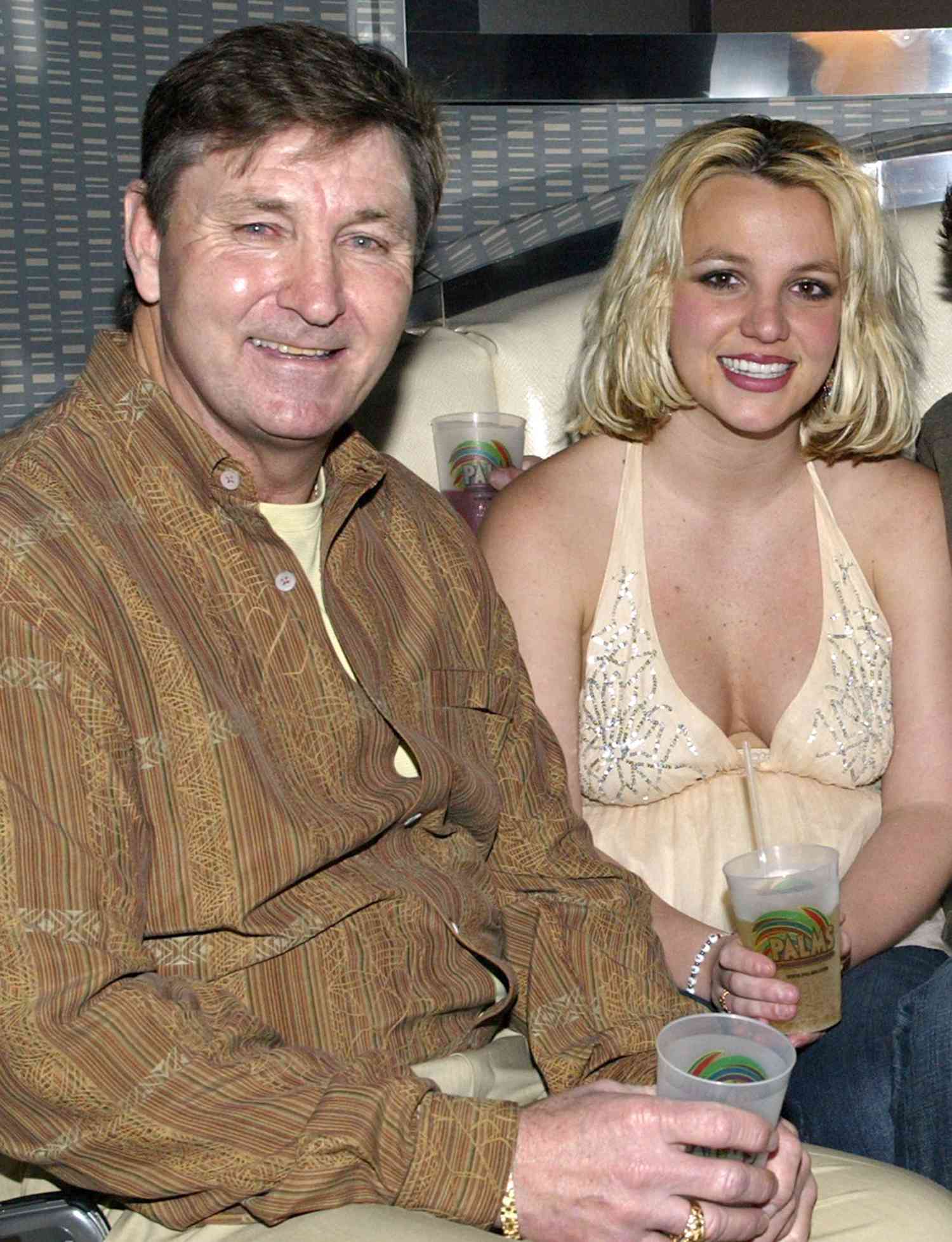
Adi Talwar Centenarian Emilia Lopez at the ArchCare Senior Life Center in Harlem, where she has been a regular for the last three years. |
One festivity was not enough for Emilia Lopez when she turned 100 this spring. She had three parties—and an excursion to an Atlantic City casino where she won $300. And no wonder. Lopez had a lot to celebrate: Not only had she reached the century mark, but she attained it while still living alone in the west side apartment she has occupied for decades.
Vivacious, scrupulous about her appearance and eager for activity, Lopez is adamant about her independence. “I can do almost everything,” she says, emphasizing that she lives alone in her own home, doing her own cooking.
Not everyone likes to cook, but by most accounts the vast majority of
older people—particularly in New York—are aging in place like Lopez. The
COVID pandemic spurred a 15 percent decline in nursing home occupancy
in the U.S. in 2020, but even before it, New York State residents were
among the least likely in the country to be in a nursing home or
assisted living facility. Nursing home occupancy rates across the state
fell to 88 percent in 2020, the lowest level in more than a decade,
according to data compiled by the Kaiser Family Foundation.
With about 1.2 million New York City residents 65 and over—and 162,000
who are 85 and up—only 41,000 people live in nursing homes in the five
boroughs.
But New Yorkers looking for alternatives to nursing
home care, particularly those with limited incomes, confront an array of
hurdles: lack of affordable housing, a shortage of safe and accessible
apartments, not enough home health care aides and waiting lists at many
programs. All but the affluent must navigate a patchwork of programs
with varying criteria and benefits. Without major policy changes, the
increase in the city’s 65 and older population—projected to surpass 1.4 million
over the next two decades—will almost certainly make it harder for New
Yorkers to age in their homes and get the help they need.
Who pays for what
Unlike
many countries, the United States does not have a long-term care
system, says Ruth Finkelstein, executive director of the Brookdale
Center for Healthy Aging at Hunter College. “We didn’t ever give it any
kind of concentrated thought.”
When most Americans think of
healthcare for seniors, they think of Medicare, the government
health-insurance program for people aged 65 and over. But while Medicare
pays for nurses and therapists providing aid, it does not cover
the more routine help given by home health care aides or long-term care
in nursing homes and assisted living facilities. People needing these
services either have to pay for it themselves or qualify for Medicaid,
the medical program for low-income people of any age. About one-fifth of
Medicare recipients also meet the stringent requirements for Medicaid.
Medicaid
then determines whether people are eligible for long-term care and/or
other services. Those who are can go into a care facility that accepts
Medicaid. If they want to remain at home, like Lopez, they can get home
health aides and other care in New York, which is more accommodating
than many other states. Unless a person is in a facility, though,
Medicaid does not provide rent assistance or food.
Howard Gleckman of the Brookings Institution has estimated
that only 15 to 20 percent of Americans receiving long-term care are in
a nursing home or an assisted living facility. But, he said in an
interview with NPR, “People are driven to nursing homes by the Medicaid
payment system. If you need long-term care, Medicaid will pay for your
room and board in a nursing home. It will not pay for it anywhere else.
So that’s an incentive for people to use nursing homes.”
Those
who don’t qualify for Medicaid have to pay for their long-term
care—wherever they receive it—themselves. Many are forced to deplete
their savings, borrow money or rely on family to do so. Assisted living
in New York City costs almost $6,000 a month, and a nursing home almost $13,000 a month, while day service (not including housing expenses) comes to about $1,950 a month.
Another problem is ensuring that the person actually gets the care he or she needs. The state requires
that people who qualify for Medicaid and Medicare enroll in a managed
long-term care plan, many of which are run by for-profit companies. The
system, some say, has led to cost overruns and some advocates question
whether the for-profit companies have an incentive to skimp on services.
Despite
the complications of providing care in a person’s home or close to it,
experts say it is worth the effort for several reasons.
One is
cost. Though estimates vary, most find that it costs more than twice as
much for someone to live in a private room in a nursing home in New York
than to stay in their own home with a home health aide.
Another
is personal satisfaction. It’s a cliché that nursing home residents
complain about the food, but their discontent often goes beyond that,
says Dheki Dolma Lama, director of transition programs for the Center for Independence of the Disabled, NY.
Patients in nursing homes, she says, often find “their personal choice
gets lost. They lose control. …Their quality of life is totally
controlled by the nursing home.”
‘A nursing home without walls’
COVID
highlighted the shortcomings of institutions, such as the difficulty of
containing infections in them, says Meghan Parker, advocacy director
for New York Association on Independent Living. People are told they
will be safer in a home, she says, but “in reality there are supports
and services available in the community that can help people remain at
home and they are often safer and happier.” The problem, she says, is
connecting people to the services they need: “It can be very
overwhelming.”
Lopez says her daughter was navigating that maze
for her when she found PACE—short for Programs of All-Inclusive Care for
the Elderly—a federal program for low-income people 55 and over who
qualify for nursing home care. Medicaid pays for her home health aide,
who does a variety of tasks that make it possible for Lopez to remain in
her apartment, including accompanying her to the grocery store and
doing her nails.
Lopez spends part of the week—these days about
12 hours—at the ArchCare Senior Life Center in Harlem. The center, run
by ArchCare, the Continuing Care Community of the Archdiocese of New
York, offers camaraderie, lunch and activities such as bingo, along with
a clinic and services like occupational therapy. ArchCare also connects
Lopez and her fellow residents with other services they might need and
keeps track of their prescriptions.
“We make all arrangements. We
try to provide everything you can imagine,” says James Williams,
ArchCare’s director of enrollment and member services, who likens the
program to “a nursing home without walls.”
Lopez says she and her
daughter are happy with the program. But they are among the fortunate
ones.“There are a lot of people who would benefit from this program but
might not qualify,” because they are not considered eligible for a
nursing home or have too much money, Williams says. And there are not
always enough spaces even for those who are eligible.
And the person needs a place to live, no small challenge in New York. A 2017 report
by the city comptroller’s office found that 39 percent of people aged
65 and over who owned their homes and 60 percent of those who rent had
to spend more than 30 percent of their income on housing, higher than
for the population as a whole.
The state government has funded some senior housing and the de Blasio administration says its Housing New York 2.0 program has produced 7,390 apartments for seniors. But demand still exceeds supply. A study
by LiveOn NY found that 44,028 older New Yorkers are on the waiting
list for affordable housing in just two Upper West Side community
districts. Those waiting lists can be seven to 10 years long.
Not
only are apartments expensive, many are not appropriate for aging
residents. The same comptroller’s report found, for example, that less
than half the city’s housing has a wheelchair accessible entrance. Older
housing—and its sometimes poor condition—can make installing even a
simple grab bar a major project. Although the city and state have
programs to assist with this, the funding has been extremely modest.
This
forces many older New Yorkers into nursing homes or poor housing
situations. Allison Nickerson, executive director of LiveOn NY, says
some city seniors live doubled up, sleeping in bunk beds.
At the
Center for Independence of the Disabled, Lama works with people thrust
into New York’s crazy real estate market when they try to leave their
nursing facility, some after years there.
These people, she says, “say they want to die in their home and it’s their right.”
Making
that move can be difficult, though. Housing, Lama says, is “the biggest
barrier. The largest percentage of people are waiting because they
don’t have a home to go to.” The city could help, she says, by
classifying people seeking to leave nursing homes as homeless, making
them eligible for certain housing assistance. So far the city has not
done that.
Selfhelp Community Service has housing for seniors –
just not enough of it. The non-profit, originally funded to help people
fleeing the Holocaust, is one provider of affordable housing with
services, a model LiveOn has praised for improving quality of life while
it “deters higher healthcare costs and prevents homelessness.”
Selfhelp
operates 11 buildings with more than 1,400 residents, who, the
organization says, live independently. The apartments are not furnished,
residents prepare their own meals and come and go as they please.
But
there are supports. “We believe our housing is not just bricks and
mortar but a way to provide services to make a house a home,” says Vice
President Sandy Myers.
The buildings feature some community
facilities and many are near other programs serving older people, such
as senior centers. Perhaps most importantly, each also has a social
worker on site who connects residents with whatever other services they
need. “They are available to do pretty much anything—even opening a can
for a resident, ” says Mohini Mishra of Selfhelp Realty Group/The
Melamid Institute for Affordable Housing. Despite that, Medicare does
not cover the cost of social workers.
Anyone 62 and over having a
low to moderate income and a household of no more than two people can
apply for an apartment. The funding for specific buildings may set
further requirements—that a person have been homeless, for example.
SelfHelp admits people with a range of needs, from those who are almost
completely independent to those who require all-day care.
Once
again, the problem is supply. The waiting lists are long and only three
of the organization’s projects are currently accepting applications.
Programs, policies and proposals
The
city and state provide a variety of services that help older New
Yorkers stay in their homes. New York City Department for the Aging
funds some 250 senior centers across the city, which reopened last month
after a long COVID closure.
The sites serve lunch—and sometimes breakfast—and offer some health
services, workshops and recreational activities. The agency also
provides money for services at selected housing developments, or in
neighborhoods that weren’t built for seniors but include a high
percentage of older people—what it calls a Naturally Occurring Retirement Community or NORC.
Another
city program, popularly known as SCRIE, freezes the rent for
low-to-moderate income older New Yorkers living in certain types of
housing. Mayoral candidate Eric Adams, who recently won the Democratic
primary, has pledged to automatically sign eligible residents up for SCRIE if he’s elected in November.
In
light of the growing need, governments at various levels are pledging
to do more. The city has announced plans to increase the number of
senior centers and provide more transportation options.. “New Yorkers
need to age in their homes and avoid institutionalization,” Alice Du,
deputy director of the city Department for the Aging, wrote in an email.
President
Joe Biden’s infrastructure plan includes $400 billion over eight years
to provide more care for seniors in their homes. The proposal does not
go into details, and as far as can be determined does not address the
many seniors who do not qualify for Medicaid but also cannot afford
long-term care, whether at home or in a facility.
Instead it
focuses on improving conditions for home health workers, who are widely
seen as vital to any effort to keep older and disabled Americans in
their homes. These caregivers—most of them women of color—make an
average of $12 an hour in the U.S. and many do not have
employer-provided health insurance. Not surprisingly, experts foresee a
looming shortage of people willing and able to do this work.
A CUNY report issued in March
found a similar situation in New York State, with home health care
workers in the city getting an average hourly wage of $15.93. The
writers recommend raising the pay to $22 an hour. While this would
require additional government spending, they argue that paying the
workers—who are mostly women, immigrants and people of color—would pump
money into the economy and save money on public assistance, which many
aides now receive to supplement their wages.
The plan would also
address the shortage of home health workers, who currently perform
taxing work for low wages. “People can do jobs that are much easier,
such as work in fast food restaurants, and make as much or more money,”
says Parker.
Advocates tried to change this equation in New York
this year by promoting the Fair Pay for Homecare Workers bill that would
have raised the pay for these caregivers to 150 percent of the minimum
wage. The bill did not get included in this year’s budget, but Parker
says the effort will continue next year.
Aside from this,
advocates have a list of things that might ease the care crunch in New
York. Much of it is centered around housing, such as more money for the
federal Section 202 program that creates homesfor very low-income older
people, rental assistance and making it easier for people to learn about
and receive help from the city’s existing rental freeze program.
Advocates
would also like to see the system tweaked so that a few people who need
part-time care could share an aide. “Now things are so siloed and so
individual. Everyone is on their own,” says Nickerson.
In
general, says Parker, there is a lot the state could do to help older
New Yorkers and others with disabilities live independently, but she
says, “We haven’t seen that in the last few budgets.”
Many
experts see a larger need to rethink the care system for older Americans
and others who need long-term care—for low-income people and also
middle-class residents who don’t qualify for Medicaid but still may not
be able to get the help they need wherever they prefer to live.
“There
needs to be a fundamental rethinking of what care looks like,” says
Nickerson. “We have to think of things very, very differently because
the model we have now doesn’t work.”