WEDNESDAY, Jan. 19, 2022 (HealthDay News) --
Homelessness is difficult enough, but when it's compounded by serious
mental health issues the result can be an inability to function at even
the most basic level.
Sometimes that leads to round-the-clock
involuntary hospitalization, and when that happens a state-appointed
psychiatric conservator can take over, making critical health care
decisions for a person deemed mentally unstable.
But new research conducted in California warns that once a conservatorship
is set up, there's a very real risk that a homeless individual will end
up stuck in a psychiatric hospital for weeks or months — far exceeding
what's needed and much longer than inpatient care provided to patients
who aren't homeless.
The bottom line, according to lead researcher
Kristen Choi, is that "our mental health care systems are falling short
in meeting the needs of individuals who are homeless at every level."
She's assistant professor in the schools of nursing and public health at
the University of California, Los Angeles (UCLA).
Taxpayers also
pay a hefty price: Choi's team estimates that it costs $767 per day
(nearly $280,000 per year) to care for a homeless person on a
psychiatric ward in California, compared to less than $14,000 to provide
them with year-round housing. Most of the patients in the study were
uninsured.
Last-resort option
In
their research, the UCLA team tracked the progress of nearly 800 Los
Angeles residents, aged 18 to 56, who were involuntarily hospitalized
within a non-profit "safety net" psychiatric facility sometime between
2016 and 2018.
A little more than half of the patients did have
housing and never ended up being placed in a conservatorship. In these
cases if they were hospitalized it was typically for less than two
weeks, Choi's team found.
But nearly half of admittees to psychiatric care were homeless. Among that group, about one in every seven were placed under a mental health conservatorship, according to the report.
Once
that step was taken, these patients often faced "very lengthy hospital
stays," averaging about five months, although some went even longer,
Choi said.
A mental health conservatorship
is "a strict legal process," she added. In California, it's a kind of
highly restricted last-resort option, intended for limited durations in
order to protect mentally impaired patients for whom "all other
treatment options have been exhausted," Choi explained.
"Mental
health conservatorships are for individuals who are 'gravely disabled'
by serious mental health illness, such as schizophrenia, bipolar
disorder, or other mental health disorders," she said. If unable to
feed, clothe or house themselves, such patients can be deemed in need of
a guardian who can step in to make mental health treatment decisions.
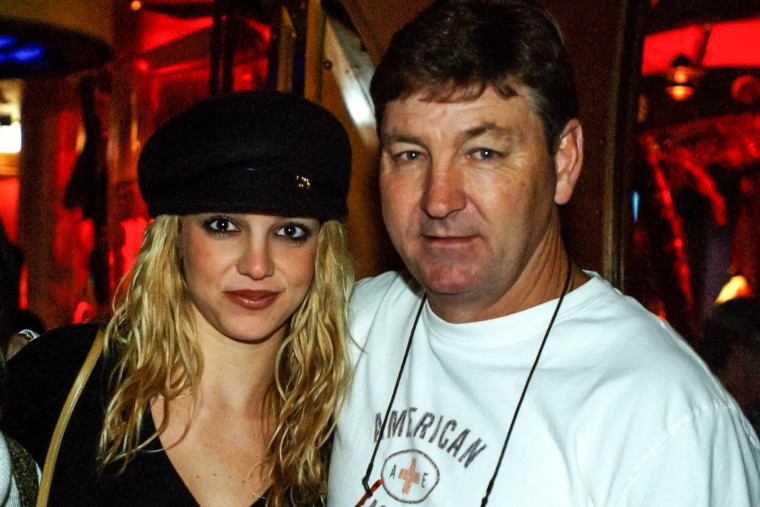
(As
such, this arrangement is not to be confused with the much-publicized
case of Britney Spears, whose conservatorship was of the financial
affairs/probate variety; the pop star never lost her ability to make her
own health care decisions.)
Once patients become stable enough,
mental health conservatorships are meant to end, with patients shifting
from an involuntary psychiatric hospital setting to a voluntary,
community-based care model instead.
But housing is crucial to that transition.
"It is difficult,
if not impossible, to stabilize mental illness for individuals who do
not have their basic needs met, including housing," Choi explained.
And
even if psychiatric stability is achieved, all patients face "a very
long waitlist for beds at lower levels of care, such as in psychiatric
step-down facilities, psychiatric rehabilitation facilities, and group
homes," she added.
That means that patients under conservatorship
often "have no choice but to wait in the hospital" after stabilization,
Choi noted, sometimes for weeks or months.
Too few options
That
wait ends up being a particularly heavy burden for homeless patients,
given that 14% of the study's homeless patients were placed in a
conservatorship compared to just 3% of patients with housing.
Overall,
even though homeless admittees to psychiatric care under
conservatorships made up just 6% of all the patients in the study, they
ended up accounting for more than 40% of the total time spent
hospitalized over the study period, the researchers found.
None of
this is good for anyone, said Choi. But she believes that "hospitals
have few options" when it comes to handling such patients, because
there's been so little progress in improving access to either housing or
community-based mental health services.
"It is important to note
that the vast majority of people experiencing homelessness do not have
mental illness," Choi stressed. "Homelessness is ultimately a problem of
lack of housing, not lack of mental health care, and we must be
cautious to not conflate homelessness and mental illness."
But she
believes that "conservatorships are not appropriate or humane for the
majority of people with mental illness," homeless or otherwise.
Hoping
to address the situation in Los Angeles, Choi said she and her
colleagues are linking street-based homeless outreach teams — such as
L.A.'s Homeless Outreach and Mobile Engagement (HOME) program — with
inpatient psychiatric services at facilities such as Gateways Hospital
and Mental Health Center.
Housing and health care
The
problem isn't confined to California, of course. Alleviating mental
illness among the homeless is an uphill battle everywhere, according to
child and adolescent psychiatrist Dr. Nicole Kozloff.
"A lack of
stable housing makes managing a serious mental illness a near-impossible
task," said Kozloff, who is associate director of the Slaight Family
Centre for Youth in Transition at the Campbell Family Mental Health
Research Institute in Toronto.
In a perfect world, mental health treatment involves psychotherapy
appointments, daily medication regimens, bloodwork, and medical
check-ups, Kozloff said. But life on the streets is far from a perfect
world.
"It is very difficult to maintain this routine if you have
to prioritize your basic needs, don't have a private place to store your
belongings, (and) can't afford transportation," Kozloff said.
"Furthermore, the stress of being homeless can exacerbate existing
mental health problems."
Kozloff agreed with Choi that solutions
lie in improved access to permanent affordable housing, coupled with a
wider availability of "mental health supports geared to a person's needs
and choices."
Choi's team published their findings recently in the online issue of Psychiatric Services.







![items.[0].image.alt](https://ewscripps.brightspotcdn.com/dims4/default/eea065d/2147483647/strip/true/crop/786x442+0+0/resize/1280x720!/quality/90/?url=http%3A%2F%2Fewscripps-brightspot.s3.amazonaws.com%2F27%2F19%2F4f0eccff41b9843889841e3355e3%2Flouisiana-supreme-court.jpg)

















