The pandemic hit everyone hard, but what implications and consequences has it had for the older generations?

Older adults have been hit hard by coronavirus disease 2019 (COVID-19). Mortality data from Oxford COVID-19 Evidence Service indicates a risk of mortality of 3.6% for people in their 60s, which increases to 8.0% and 14.8% for people in their 70s and over 80s.1 An age-related mortality study from China showed that patients of COVID-19 above aged 55 years had 3 times increased mortality. Older individuals are much more likely to develop COVID-19 related complications.2 The increased mortality reflects the underlying biological, social, and psychological vulnerabilities faced by the older population. Elderly individuals are also disproportionately affected by social distancing policies and other restrictions to stop the spread of the virus, resulting in increased loneliness, social isolation, and loss of freedom and support networks.3
Over the course of the pandemic, we have seen considerable media coverage about the risk of COVID-19 to older people. Unfortunately, much of this discourse has negatively fueled an already existing ageist sentiment. Ageism, which some define as stereotyping, prejudice, or discrimination toward people on the basis of age, is a serious international concern with important health implications.4 Multiple studies have indicated that ageism toward older adults is highly prevalent across countries and continues to grow with global population aging.5 Negative attitudes toward older adults pose significant risks to the health and well-being of older individuals, such as higher mortality risk, poor functional health, slower recovery from illness, and poor mental health.6
Negative attitudes toward this population are particularly prevalent on social media. A Twitter analysis of 18,128 tweets between March 12 and March 21, 2020, showed that about one‐quarter of all tweets could be considered ageist, either because they included jokes or ridicule aimed at older adults or because their content downplayed the relevance of COVID‐19 and/or implied their lives were less valuable.7 Ageist attitudes are nothing new. A previous study of Facebook posts indicated that 74% excoriated older individuals, 27% infantilized them, and 37% advocated banning them from public activities, such as shopping.8 Various social media discourses have surfaced about prejudiced representation and denigration of older people in society. For example, COVID-19 has been characterized with the hashtag #BoomerRemover, which has been trending on social media platforms, often accompanied with ageist disparaging and devaluing memes.9
Public discourse during the pandemic has increasingly portrayed those over the age of 70 as helpless, frail, and unable to contribute to society. These views are being spread by social media, the press, and public announcements by government officials throughout the world. There has been considerable media coverage and online discussions about potential for rationing of care of elderly people as they are more expendable than persons in other age groups. Some of the coverage seems to suggest that the deaths of older people somehow are not as important as the younger population.10
There have been numerous examples of flagrant discrimination against older individuals during COVID-19. Earlier in its course, COVID-19 was believed primarily to affect elderly people. Many young people did not follow adequate precautions, and strong public health warnings were not issued. Even after COVID-19 outbreaks in many nursing homes, Centers for Disease Control and Prevention (CDC) guidelines did not identify residents in long-term care as a high priority for testing.11 Treatment resources and personal protective equipment have been consistently directed toward the younger population.12 In a press briefing in March, World Health Organization Director-General Tedros Ghebreyesus took unnamed nations to task for failing to treat the death of older adults as a “serious issue” and exhibiting signs of “moral decay.”13
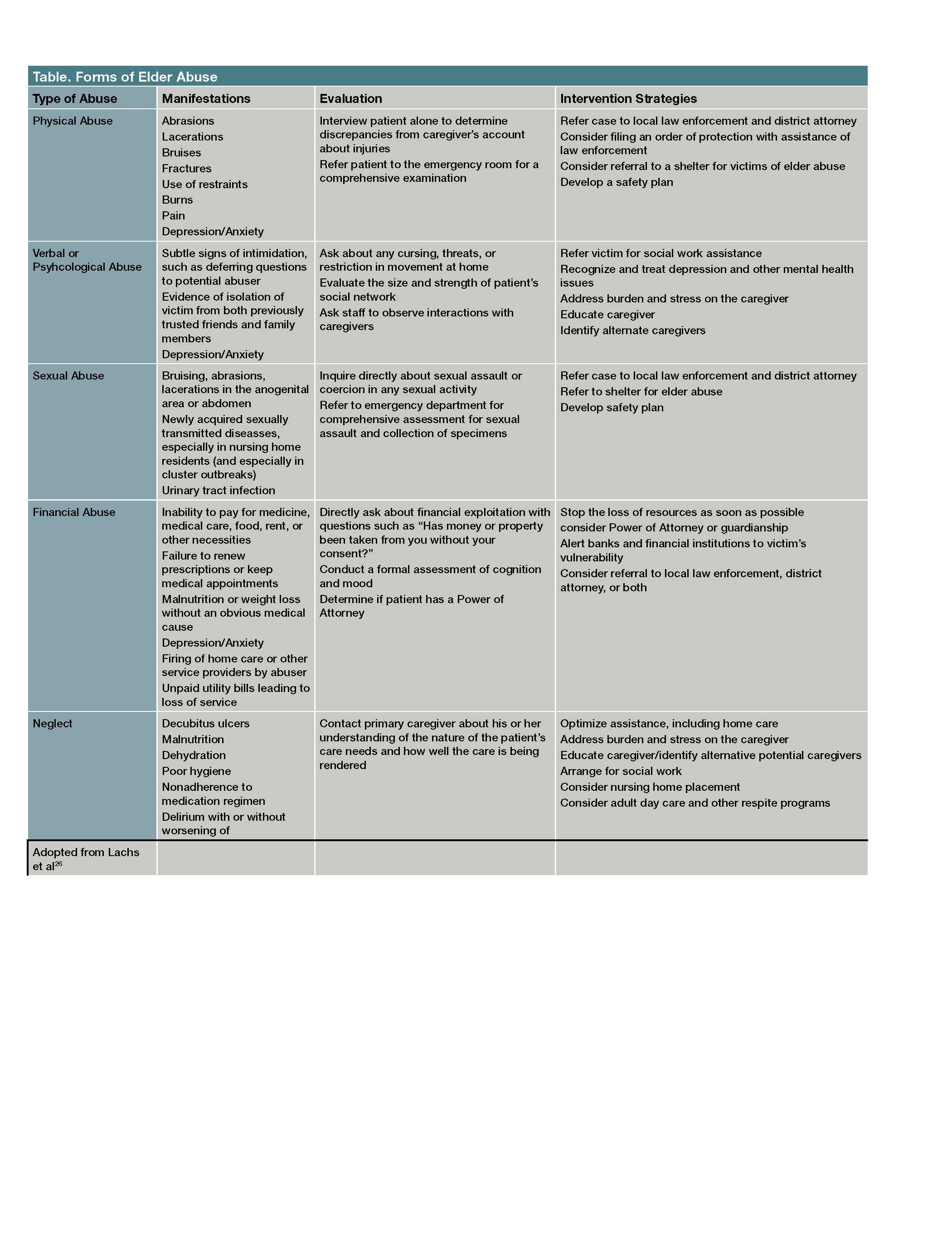
One of the disturbing social consequences of COVID-19 includes a significant increase in the number of elder abuse cases, paralleling the rise of ageism. The CDC defines elder abuse as an “intentional act or failure to act by a caregiver or another person in a relationship involving an expectation of trust that causes or creates a serious risk of harm to an older adult.”14 Elder abuse was a huge public health problem globally even before COVID-19. It is estimated that in the United States, approximately 1 in 10 individuals over the age of 60 suffers physical, verbal or sexual abuse, or financial exploitation.15
Elder abuse is significantly underreported. Only 1 in 24 cases may be reported.16 In almost 60% of elder abuse and neglect incidents, the perpetrator is a family member.17 Social isolation is a significant risk for elder abuse. Other risk factors include cognitive impairment, physical frailty, and dependence on others for care. Nursing home residents are also particularly vulnerable to elder abuse.18 All of these risk factors have been compounded by COVID-19.
To reiterate, since the start of the COVID-19 pandemic, there has been a massive increase in the reports of elder abuse. Reports range from incidents of family violence, neglect, and financial scams. The Federal Trade Commission and the American Bar Association as well various state departments have issued warnings to the public.19 In Europe, there have been distressing reports of older people abandoned in care homes in Spain.20 In Italy, where 23% of the population is aged 65 years or older, some hospitals have used chronological age-based cutoffs to ration ventilators.20
Systemic issues
Mortality data from the Oxford COVID-19 Evidence Service indicates a risk of mortality of 3.6% for people in their 60s, which increases to 8.0% and 14.8% for people in their 70s and 80s.
Not only do pervasive ageist attitudes and stereotypes contribute to negative health outcomes, but ageism among health care professionals can also result in discriminatory practices that place older people at risk.21 Studies have found widespread negative attitudes toward older people and old age among physicians, medical students, and nurses.22 Such attitudes can lead to practical consequences for older patients. For example, assumptions regarding functional and cognitive decline can lead to more limited provision of medical information, withholding certain treatment options, and exclusion from clinical trials.23 Ageist attitudes have also been found among mental health practitioners and trainees (such as assuming that depression symptoms are normal among elderly adults), which in turn may restrict access to treatments and contribute to functional decline.24
Unfortunately, many well-intentioned efforts to combat the effects of COVID-19 have also resulted in marginalization of elderly adults. For example, recent shift towards telemedicine excludes roughly half of the adults over age 65 in the United States who lack access to broadband services.
Concluding thoughts
Elder abuse and ageism are extremely hard problems to combat. There are no clear ways to reduce ageism and change attitudes toward aging. Combined interventions with education and intergenerational contact seem to show the largest effects on attitudes.21
Adult Protection Services (APS) run by local or state health departments are usually responsible for investigating cases of elder abuse. However, few financial resources, insufficient access to information needed to resolve elder abuse cases, inadequate administrative systems, and lack of cross‐training with other disciplines in the aging field serving clients with mental health disabilities—these have hindered the role of APS workers in intervening in abusive situations.25
Two important federal laws address the issue of elder abuse: the Older Americans Act (OAA) and the Elder Justice Act (EJA). However, lack of funding and relaxed enforcement have diluted their effectiveness. The EJA has received less than 10% of the funding that was authorized, especially with respect to achieving its main goal of dedicated funding for APS.25 Denial of elder abuse and lack of funding continues to be a significant problem in the enforcement of existing laws. Urgent policy changes are needed to strengthen the protections for the elderly during COVID-19.
Dr Malik is a Professor in the Department of Psychiatry at Johns Hopkins University SOM. Dr Burhanullah is an Associate Professor in the Department of Psychiatry, Johns Hopkins University SOM. Dr Lyketsos is the Elizabeth Plank Althouse Professor and Chairman of the Department of Psychiatry, Bayview Campus, Johns Hopkins University SOM.
References
1. Oxford COVID-19 Evidence Service (2020). Global COVID-19 case fatality rates. Accessed September 25, 2020. https://www.cebm.net/oxford-covid-19-evidence-service/
2. Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect. 2020;80(6):14-18.
3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. Accessed September 18, 2020. https://jamanetwork.com/journals/jama/fullarticle/2762130
4. Butler RN. Ageism. In: Maddox GL, ed. The encyclopedia of aging. Vol. 1: A–L. New York, Springer Publishing; 2000:38–9.
5. North MS, Fiske ST. Modern attitudes toward older adults in the aging world: a cross-cultural meta-analysis. Psychol Bull. 2015;141(5):993–1021.
6. Chang ES, Kannoth S, Levy S, Wang SY, Lee JE, Levy BR. Global reach of ageism on older persons’ health: A systematic review. PLoS ONE. 2020;15(1):e0220857. Accessed September 18, 2020. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0220857
7. Jimenez‐Sotomayor MR, Gomez‐Moreno C, Soto‐Perez‐de‐Celis E. Coronavirus, Ageism, and Twitter: An Evaluation of Tweets about Older Adults and COVID‐19. J Am Geriatr Soc. 2020;68(8):1661-1665.
8. Levy BR, Chung PH, Bedford T, Navrazhina K. Facebook as a site for negative age stereotypes. Gerontologist. 2014;54(2):172‐176.
9. Ayalon L. There is nothing new under the sun: ageism and intergenerational tension in the age of the COVID-19 outbreak. Int Psychogeriatr. 2020;1‐4. Published online April 14, 2020.
10. Ayalon L, Chasteen A, Diehl M, et al. Aging in Times of the COVID-19 Pandemic: Avoiding Ageism and Fostering Intergenerational Solidarity. J Gerontol B Psychol Sci Soc Sci. 2020. Published online April 16, 2020.
11. Overview of Testing for SARS-CoV-2 (COVID-19). CDC. Updated September 18, 2020. Accessed September 25, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html
12. Mahr J. Short staffing. PPE shortages. Few inspections. Why calls are growing for Illinois nursing home regulators to step up efforts on COVID-19. Chicago Tribune. May 13, 2020. Accessed September 18, 2020. https://www.chicagotribune.com/coronavirus/ct-coronavirus-illinois-nursing-homes-regulators-pritzker-20200513-3bdofjnaivhadg2yt7kcf2psm4-story.html
13. Carbonaro G. ‘Every life matters’: WHO chief warns against COVID-19 age discrimination. CGTN. March 11, 2020. Accessed September 18, 2020. https://newseu.cgtn.com/news/2020-03-11/-Every-life-matters-WHO-warns-against-COVID-19-age-discrimination-OKDSHuH0gU/index.html
14. Elder Abuse. CDC. Accessed September 18, 2020. https://www.cdc.gov/violenceprevention/elderabuse/index.html
15. Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health.2010;100(2):292-297.
16. Lifespan of Greater Rochester Inc, Weill Cornell Medical Center of Cornell University, New York City Department for the Aging. Under the Radar: New York State Elder Abuse Prevalence Study. May 2011. Accessed September 18, 2020. https://ocfs.ny.gov/main/reports/under%20the%20radar%2005%2012%2011%20final%20report.pdf
17. Amstadter AB, Cisler JM, McCauley JL, Hernandez MA, Muzzy W, Acierno R. Do incident and perpetrator characteristics of elder mistreatment differ by gender of the victim? Results from the National Elder Mistreatment Study. J Elder Abuse Negl. 2011;23(1):43-57.
18. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5). https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(20)30061-X/fulltext
19. Tressler C. Coronavirus: Scammers follow the headlines. Federal Trade Commission Consumer Information. February 10, 2020. Accessed September 18, 2020. https://www.consumer.ftc.gov/blog/2020/02/coronavirus-scammers-follow-headlines
20. Minder R, Peltier E. A deluged system leaves some elderly to die, rocking Spain’s self-image. NY Times. Updated March 29, 2020. Accessed September 18, 2020. https://www.nytimes.com/2020/03/25/world/europe/Spain-coronavirus-nursing-homes.html
21. Burnes D, Sheppard C, Henderson CR Jr, et al. Interventions to Reduce Ageism Against Older Adults: A Systematic Review and Meta-Analysis. Am J Public Health. 2019;109(8):e1‐e9. Accessed September 18, 2020. https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2019.305123
22. Chrisler JC, Barney A, Palatino B. Ageism can be hazardous to women’s health: ageism, sexism, and stereotypes of older women in the healthcare system. J Soc Issues. 2016;72(1):86–104.
23. Briggs R, Robinson S, O’Neill D. Ageism and clinical research. Ir Med J. 2012;105(9):311–312.
24. Bodner E, Palgi Y, Wyman MF. Ageism in mental health assessment and treatment of older adults. In: Ayalon L, Tesch-Römer C, eds. International Perspectives on Aging. Cham, Switzerland, Springer Nature; 2018;19:241–262.
25. Blancato B. It’s time to make the Elder Justice Act more effective. Forbes. August 14, 2019. Accessed September 18, 2020. https://www.forbes.com/sites/nextavenue/2019/08/14/its-time-to-make-the-elder-justice-act-more-effective/#6b87f7e45605
26. Lachs MS, Pillemer KA. Elder Abuse. N Engl J Med. 2015;373(20):1947-1956.

No comments:
Post a Comment