Thursday, December 31, 2020
102 Year-Old Woman Beat the 1918 Flu and Now Has Beat COVID --- TWICE!
And now, the 102-year-old New York resident just did it again. She survived a second coronavirus diagnosis, according to her daughter, Joanne Merola, who spoke to CNN affiliate WPIX.
"My invincible mother tested negative," Merola said.
Full Article and Source:
She's 102. She lived through the 1918 flu and now she's beat coronavirus — twice
93 Year-Old Woman Gets Diploma 75 Years After She Was Forced to Quit High School
A 93-year-old senior citizen from Centerville, Virginia named Eileen Delaney was one of many people to not finish high school back in her day. However, this has recently changed. For her 93rd birthday around a week ago, she received a bit of a surprise—a gift in the form of a high school diploma from the school she attended and quit 75 years ago.
So, 93-year-old Eileen Delaney has finally received her high school diploma from Port Richmond High School in Staten Island, New York—the school she had attended 75 years ago and was unfortunately forced to quit so that she could get a full-time job which would help pay the bills.
You see, Eileen’s mother passed away when she was but 12 years old. Her father remarried when she was 14. Making ends meet was hard, so she got a job at the New York Telephone Company—a job she quite enjoyed. And she might not have graduated school back then, but she kept in touch with all of her friends there.
Eileen’s niece got in touch with the principal of Port Richmond High School, the school Eileen attended 75 years ago, as well as the alumni association, which Eileen was a part of throughout the years, and managed to get her a high school diploma from the class of 1945.
Needless to say, Eileen was absolutely surprised—she never would have guessed that she’d get a diploma for her birthday, let alone her 93rd! It has been 75 years since she left school, after all.
Full Article and Source:
93 Y.O. Virginia Woman Gets Diploma 75 Years After She Was Forced To Quit High School
92 Year-Old Woman With Dementia Performs "Moonlight Sonata" on Piano
92-year-old pianist is wowing her audience. Elaine Lebar suffers from dementia but remembers her love for music.
She recently went viral on TikTok with a performance of Beethoven's 'Moonlight Sonata' in 2019.
Full Article and Source:
92-Year-Old Woman With Dementia Performs 'Moonlight Sonata' on Piano
Wednesday, December 30, 2020
Walt Disney's Grandson Fighting Courts And Twin For His Inheritance
Last June, Cowan allegedly said in court: "Do I want to give $200 million dollars effectively to someone who may suffer from Down syndrome? The answer is no." Lund's DNA test proved he did not have Down syndrome and he is able to manage his own finances.
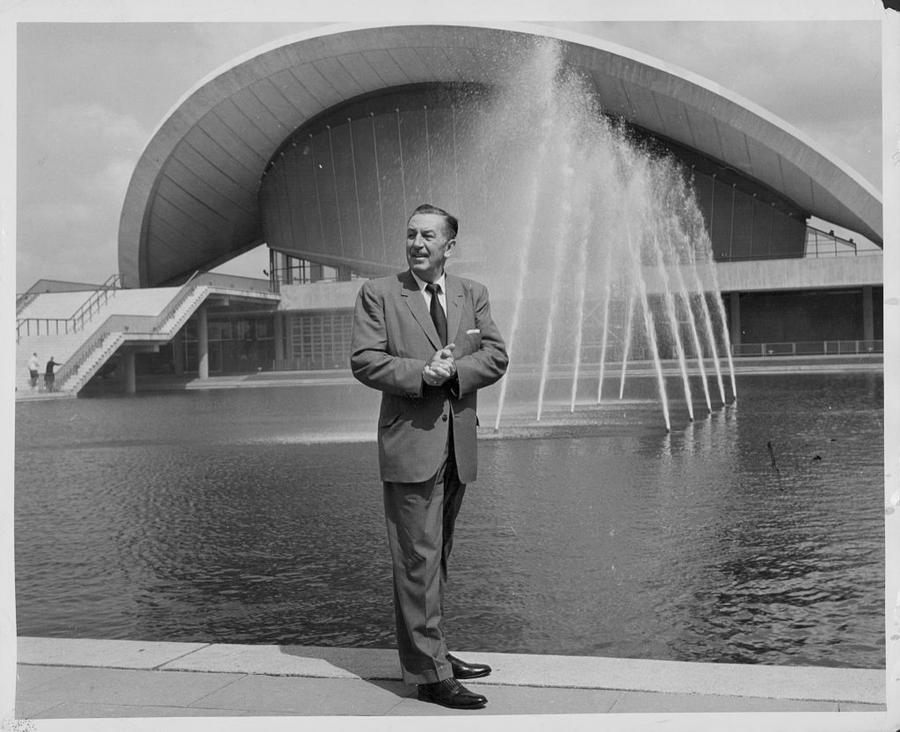
Photo by Express/Archive Photos/Getty Images
Walt Disney died in 1966, four years before Bradford and his twin sister Michelle were born. He left a significant part of his fortune to his daughters Diane and Sharon and their descendants. Bradford and Michelle's mother Sharon died in 1993 after a battle with breast cancer. She left her kids a portion of her estate when they turn 35 with the caveat that three appointed trustees have to find them mentally capable in order for them to receive their trust funds. Sharon's will stipulated that Bradford and Michelle would receive payouts from their trust fund on their 35th, 40th, and 45th birthdays. She appointed the trustees which included her husband Bill, her sister Diane, and a real estate agent who scouted the location for Disney World. The trustees each receive $1 million a year until Bradford and Michelle's payments were made.
When the twins turned 35, the trustees decided Bradford lacked the mental capabilities necessary to receive his payout. Michelle, on the other hand, was awarded her payout, despite allegedly being a drug addict and after a nearly fatal brain aneurysm in 2009 that reportedly affected her mental capabilities. Bradford and Michelle were once close siblings. Now, they've been battling over their $400 million inheritance and haven't spoken in four years. Bradford's side of the argument is that Michelle suffered brain damage from her aneurysm and that the trustees control Michelle like a "robot," yet she gets the payouts from their shared trust fund. Michelle's side includes the trustees, and their argument is that Bradford is mentally incompetent. The feud started on Labor Day 2009 when Michelle had her near-fatal aneurysm. As she fought for her life, her father tried to move her to Arizona where he lived with his fifth wife and Bradford. The trustees filed suit to stop him and Michelle chose their side when she recovered. Further complicating matters is the fact that the twins' aunt Diane and their half-sisters worry that Bradford was being used by his father and his step-mother Sherry for his money. In a lawsuit filed in Maricopa County, Arizona, Diane and the siblings called him a virtual captive in his home. Bradford has denied this.
Now Bradford is taking issue with how the caveat in his mother's will is being interpreted. He and his attorneys claim the probate system is susceptible to corruption. Basically, the longer the client is considered incapable of managing his or her affairs, the longer the trustees get paid.
Judge Cowan removed himself from the Bradford Lund case. He also is no longer a sitting judge in probate court.
Now disbarred, former Weld District Court judge’s misconduct described in new court documents
Ryan Kamada disbarred this week by the Office of Attorney Regulation Counsel for the Colorado Supreme Court
 |
| GREELEY, CO – JULY 21:The Weld County Courthouse stands near downtown at the Weld County Centennial Center in Greeley July 21, 2020. (Alex McIntyre/Staff Photographer) |
By Trevor Reid
Ryan Kamada, the former Weld District Court judge who pleaded guilty earlier this year to a federal felony charge for obstructing an investigation into a local drug trafficking ring, was disbarred this week by the Office of Attorney Regulation Counsel for the Colorado Supreme Court.
Documents from the office’s proceedings show Kamada’s misconduct was not limited to his leaking details about the 2019 investigation to a friend who was involved. Kamada was appointed as a Weld County magistrate in May 2015. During that time, he maintained long-running text message chains with his friends, according to court documents.
 |
| Ryan Kamada, after taking the bench in 2015 as a Weld County magistrate. (Greeley Tribune file photo) |
In September 2016, Chacon asked Kamada to look up information about someone. Kamada responded to the man in question “wasn’t convicted of the sex assault but he was on other charges and ended up in (expletive) prison man.” The text went on to say the man in question was having sexual relations with a minor and giving her cocaine.
“If that kid lives I’ll be shocked,” he wrote.
In March 2018, Kamada discussed a pending dependency and neglect case in the group chat. A friend asked whether the parent involved had a warrant, and Kamada said he didn’t find one but he hadn’t checked hard, according to court documents.
The next day, that same friend sent a group chat a photo of two children who were reported missing. Kamada went on to talk about details of the family, including that the mother was found overdosed.
On Jan. 8, 2019, then-Gov. John Hickenlooper appointed Kamada to succeed Elizabeth Strobel as Weld District Court judge. That same month, Chacon asked about someone taken into custody by the Federal Bureau of Investigation. Kamada tried looking up the case, but could not find it. He surmised it was a federal case, according to court documents.
Also that month, Kamada presided over a divorce proceeding and sent a photo of the first page of the decree of dissolution to his friends. Kamada said he was “going to grant this today so she is free game tomorrow night,” court documents state.
Kamada also told a friend he had the friend’s brother-in-law in court, including a photo of a party involved in a custody battle. The photo was not the friend’s brother-in-law. Still that same month, Kamada sent the group a photo of a father and a child, saying, “check out the dad in my trial today.”
Finally, court documents noted Kamada’s leak about the 2019 drug trafficking investigation involving Alberto “Beto” Loya. Loya was sentenced in June to serve 10 years in prison after pleading guilty to conspiracy to possess with the intent to distribute a controlled substance, a Class 1 drug felony, and conspiracy to money launder, a Class 4 felony. He originally faced 21 charges but made a plea agreement with prosecutors.
Kamada resigned from the district court judge position a day before Greeley police announced Loya’s indictment and the arrest of some of his associates. A few days later, he formed Kamada Law, LLC, in Windsor. He took a job the following month with Burnham Law. In March, according to Kamada’s LinkedIn profile, he left Burnham Law for Kamada Law.
Kamada signed an agreement consenting to disbarment and accepting the facts laid out in the court documents. The agreement requires that he pay $224 to the Colorado Supreme Court Attorney Regulation Offices for costs incurred in the case.
Kamada is free on bond until his sentencing 2 p.m. Dec. 4. Court records indicate he likely faces 12-18 months of imprisonment and no fines. He faces at least one year of supervised release and no more than three years.
Elderly care task force disbanded before new DA takes office, CAVE director says
In a letter Tuesday, CAVE Director William Loomer announced that the task force will be disbanded effective Wednesday.
New District Attorney Jared Williams said Loomer was not authorized to close the task force by anyone in his incoming administration.
"If he was authorized to do so, it could have only come from the current administration. I do not take office until Jan. 1, 2021, and my team will be assessing all programs after that time," Williams said in a statement.
Williams, whose term begins Monday after he beat Republican incumbent Natalie Paine on Nov. 3 with 50.51 percent of the vote, shared with The Augusta Chronicle a Dec. 28 email exchanged between Loomer and himself. In those emails, Loomer told Williams he was planning to leave the position and felt Williams should let him know his plans for the task force.
Williams responded by telling Loomer to talk to Chief Michael Lanham and Investigator Samuel Long about the status of the task force's caseload. Williams indicated he wanted to work together to make sure the community's needs are met. Williams said the email exchange was the last conversation the two had about the future of the task force.
Paine said the decision to disband the task force was the only choice the CAVE team had. She claims all the people who run the task force were told to leave and when attempts were made to transition to a new team, if there is one, they were declined.
Loomer said state legislation requires the district attorney of a circuit be responsible for creating or maintaining teams such as CAVE. He said Williams has offered no transition strategy and indicated he intends to restructure the employment status of CAVE leadership.
"It is in the public interest that the public be notified that the Task Force is no longer a resource available to them. I sincerely hope that the incoming administration continues to serve the vulnerable and elderly in a way that fits their model," Loomer said in the letter. "My offer to help the new administration with this remains in place."
 |
| New District Attorney Jared Williams |
"I want to personally thank every single member of this phenomenal team for their hard work, dedication and desire to help the most under-served demographic in our community – the elderly and disabled. The officers and staff were a torch in the darkness for so many forgotten victims," Loomer said in the letter. "I would also like to thank our partners from different agencies who made our mission possible and recognized the importance of this work."
The current cases will be transferred to other personnel in the district
attorney's office, while the Facebook page will start to post resources
and other tools for the public to use to protect themselves and others,
Loomer's letter said.
Tuesday, December 29, 2020
Man placed in guardianship by family who objected to new wife fights to get rights restored
ORLANDO, Fla. — A retired engineer put into a professional guardianship years ago at the request of his family is pleading to get his rights restored.
But even after a board-certified licensed Florida psychiatrist says he’s capable of caring for himself, legal challenges have prevented the doctor’s opinion from even being considered.
Doug Keegan’s guardianship case started in 2014.
For the past two years, he’s been living in an extended stay hotel. Before that, Keegan lived in locked-down dementia units at assisted living facilities.
He physically broke down the door at one of those facilities and was moved into the hotel as a last resort, according to his guardian’s attorney.
“This is the kitchen. It’s small, but it’s got a microwave and toaster oven,” Keegan said, giving the I-Team a tour of his small room.
Keegan has a copy of Florida’s guardianship statute attached to his refrigerator.
His ride to the courthouse is parked by the door.
“My transportation’s my bike. Occasionally I take the bus,” he said.
And binders stacked near his laptop computer contain copies of legal pleadings Keegan sent to judges.
“This is probably where I spend 80 percent of my time. So I work on my laptop,” Keegan said.
“He doesn’t understand anything you say”
Keegan’s not legally allowed to advocate for himself.
“Mr. Keegan can’t do that. He doesn’t have any rights,” said attorney H. Kyle Fletcher.
Fletcher represents Keegan’s guardian and is paid $350 an hour from Keegan’s funds.
“He’s incapacitated. Which means he actually doesn’t understand anything you say,” said Fletcher.
But in September, Judge Alan Apte questioned that, after Keegan filed a 12-page report pleading for the removal of his guardian.
“I set this hearing because I believed you had some capacity,” Judge Apte said in the hearing.
Keegan told the court he “absolutely” had capacity, but his guardian’s attorney disagreed.
“I’m just trying to tell the court he does not have mental ability to understand logic,” Fletcher said.
“He doesn’t grasp what the judge is saying, if you understand what I’m saying,” Fletcher explained in a Zoom interview.
“The guardian’s attorney wanted to appoint a court-appointed attorney, which I knew would be useless. I said no, no. I want my own attorney. And so (Judge) Apte said do you know anyone? I said yeah, I know this Leslie Law,” Keegan said.
Keegan met attorney Leslie Ferderigos through a guardianship reform Facebook group.
“He found a Nigerian woman to marry off of Craigslist”
"He’s clearly got capacity. He’s been involved in this for six years. And he has tried multiple times, including from himself, to get out of this,” Ferderigos said.
Keegan’s guardianship started after he married a woman from Kenya who his family believed was financially exploiting him.
“He found a Nigerian woman to marry off of Craigslist… the in-person Nigerian scam,” said Fletcher.
Contrary to Fletcher’s assertion, Keegan says it was a legitimate marriage.
“I had known her for a year. I brought her to my Mom’s house for Christmas dinner the year before,” Keegan said.
We spoke to her from Kenya, where she was visiting family over the Christmas holiday. She said she first came to the United States in 2002 and became a citizen in 2009. She also characterized her marriage to Keegan as legitimate.
Keegan’s family also sought guardianship because he had a history of alcohol abuse, which led to him being hospitalized.
“I have a problem with alcohol, which is irrelevant to guardianship. You can be a gambler, you can be morbidly obese. You can have a million problems. That’s not a reason to say put him in guardianship, because he may hurt himself,” said Keegan.
One doctor who evaluated him in 2014 said his drinking “doesn’t rise to the level of guardianship”.
But months later, a judge declared Keegan incapacitated.
“They went in there and they stripped me of all my rights. They took all my money. Took all my rights away from me,” Keegan said.
“He’s living in a motel with no supervision”
Keegan and his older brother told us he finished first in his class in high school and college.
He worked as an electrical engineer and contracted with power providers, regulators and other large companies on projects all over the world.
Keegan’s lucrative consulting work enabled him to buy a condo with cash and retire early.
Now, more than $200,000 he saved has gone to pay guardians and attorneys, but Keegan is only allowed to shop at certain places with a restricted debit card.
“I’m allowed Denny’s, McDonald’s, Subway, Golden Corral, Chick Fil-A. and then there’s a Dollar Tree I can go to,” he said.
Attorney Fletcher told Judge Apte the restrictions are intended to prevent Keegan from purchasing alcohol.
“They have him in a plenary guardianship stating that he has no capacity to have any of his normal rights, but he’s living in a motel with no supervision,” said Ferderigos.
In explaining why Keegan is in a plenary guardianship, which is the most restrictive type of guardianship in which a person retains no rights, Fletcher said it’s because he was diagnosed with frontal lobe dementia by a psychiatrist in 2015.
The Mayo Clinic says that to diagnose frontal lobe dementia, doctors should use blood tests, sleep studies and brain scans to diagnose frontal lobe dementia.
But the doctor’s report doesn’t indicate he did any of that.
In his report, that doctor indicated he conducted the exam in Keegan’s home and did not talk to his family physician.
“That diagnosis was very suspect, based only on a very cursory examination,” said Dr. Sam Sugar, who is a retired internal medicine doctor.
Sugar founded Americans Against Abusive Probate Guardianships and has known Keegan for three years.
“There’s no evidence now he suffers from any kind of dementia. So it’s imperative that the court understand people can recover, they can get better and they no longer need the guardianship,” said Sugar.
Judge Apte signed an order allowing Keegan to be evaluated by a psychiatrist from Boca Raton, FL.
That doctor determined Keegan had full capacity.
Attorney Fletcher objected to not being properly notified and got a hearing with a different judge, who overturned the doctor’s appointment and appointed the doctor Fletcher recommended to evaluate Keegan.
“They’re contesting the doctor’s report because he didn’t get evaluated by the doctor they wanted him to be evaluated by,” said Ferderigos.
“That’s the modus operandi of this lawyer who goes around in other cases doing the same thing. Finding someone she wants, rather than what the parties agree upon or who’s on the appointed list,” said Fletcher.
“If the judge rejects it out of hand because he’s not on some list, I think that tells you everything you need to know,” said Dr. Sugar.
“Anyone in a high level of government should be horrified”
“Dr. Sugarman (SIC) seems to me to be a bizarre person who absolutely has no idea what goes on in the law,” said Fletcher.
Keegan’s attorney requested another hearing with Judge Apte.
At that hearing he picked a physician to evaluate Keegan from among six physicians offered by the two sides.
That was after Dr. Sugar sent the judge a letter asking the judge to “grant Mr. Keegan a full and comprehensive re-evaluation with an independent, third party fully qualified physician.”
“After all, what’s at stake but a man’s life? No big deal,” said Sugar.
“He’s probably about as competent as Mr. Keegan,” said Fletcher, when asked about Sugar’s letter to the judge.
“It’s horrible. Anyone in a high level of government should be horrified with what they’re seeing here in the courts,” said Keegan.
Keegan is expected to be evaluated by the new doctor next month.
If you have a story you’d like the I-Team to investigate, email us at adam@abcactionnews.com
Former Weld County judge who tipped off friend about drug investigation is censured
According to the censure, Ryan Kamada also frequently texted his friends inappropriate comments about what was happening in his courtroom
The Colorado Supreme Court on Monday publicly censured a former Weld County District Judge who tipped off his friend that their mutual acquaintance was the target of a federal drug investigation.
Ryan Kamada was censured for violating a variety of ethical and professional rules, The Denver Post reported.
“Then-Judge Kamada’s pattern of reckless disregard for confidential information undermined his office and the public’s confidence in the judiciary,” the censure reads. “In fact, his behavior interfered with a multi-agency law enforcement operation and resulted in a criminal conviction in federal court.”
Kamada tipped off his friend after learning about the investigation when officers asked him to sign a search warrant. He warned the friend via text to stay away from the acquaintance because of the investigation. The friend then tipped off the acquaintance.
Despite Kamada’s warning, both men were later arrested as part of the drug investigation.
According to the censure, Kamada also frequently texted his friends inappropriate comments about what was happening in his courtroom, alerting one friend to a finalized divorce and telling the friend the woman would be “free game tomorrow night.”
Kamada resigned in August 2019 and pleaded guilty to a federal felony
charge of obstructing an investigation. He was disbarred and will be
sentenced in the federal criminal case in February.
A Small Glimpse of a Nursing Home Employee’s Life
(EDITOR’S NOTE: As the number of positive cases skyrockets at Keyser’s Piney Valley Nursing Home, an employee there wrote this piece to help the public better understand how they struggle every day to continue to give their residents the best care possible amidst the relentless pandemic. What follows are entirely her words.)
By Kendra Keplinger
We wake up, stumbling to our morning rituals and hoping our nightmares haven’t come true. Staring in the mirror while brushing our teeth, a weary expression glances back at us. Wrinkles darken underneath the eyes. Our noses red with minor abrasions from two layers of masks. A thin red line runs across our foreheads from the safety goggles.
On our way to work, we try to lighten any mood through the sounds of the season on the radio and whispered prayers, knowing it’s been anything BUT “holly” and “jolly.”
Upon arrival, we put our cloth mask on, sanitize our hands before entering the building, and go to our cubby. We switch out into our N95 and surgical masks followed by a shield or goggles (tightened so it lessens the fog…but not entirely.)
We’re briefed about deaths the night before, and it’s not uncommon to hear of even more disheartening news already unfolding. Still, we swallow our tears and go about our day with the best attempt of a smile we can manage.
Our residents are tired, their cabin fever continues to spike, and they’re disgruntled with the pandemic, some fearful. Still, most manage to find the good in each day as we continue to pray it’ll pass.
Some have appetites. Others are diminished. Most wonder when they’ll see the ones they love or old roommates they once had before chaos struck. They can’t help but wonder, “What next?” We cautiously do the same.
Families gather outside of bedroom windows, watching the live action horror film of their loved one paying the price of the pandemic. They cannot hold their hands or kiss them goodbye. They have to stand by and helplessly watch, but they do so out of love in the winter weather to be a presence when their resident needs them most. Their devotion and love unending.
From inside the room, the pain lingers from a new perspective. We feel the personal guilt of being able to hug them and hold their hands when the family cannot. We see the silent tears of the passing resident, weeping in their sleep. We hear the death rattles. We see the forced rise and fall of their chest, fighting its last fight to continue functioning. Their frequent jolts before the morphine cause us to jump as well. We check the pulse and respirations and watch them raise and lower. The tent goes up and provides a cryptic view of what looks like a graveside service from the coffin’s point of view. Once the tent is fully covered, it transforms into a miniature theatre with a private screening of the family’s worst nightmare. Each take turns walking up toward the window in hopes to let the resident know they’re there. The grief in their eyes and tears that follow sting ours as well. We want to take a folding chair, bust out the window, and allow them the last few moments with their loved one as the clock continues ticking, but that’s not acceptable even in such extenuating circumstances.
It’s time for the changing of the caregivers. The next post has arrived to console the resident and family. It takes everything to stand up and walk out of the room because we know we won’t see them when we come back. Passing down the hall, we see the emotional and physical despair on the residents. We just wish we could make it disappear into thin air, but we can’t. Only time can, but we don’t have much of it.
Clocking out and taking a deep breath of air before switching into our cloth masks, we take a second and sigh. The battle isn’t over. Some say it should remain in the building, but it stays with the residents in our hearts. We carry it home weary and tired to a world who cares but doesn’t truly understand what we’ve experienced. Those that embrace us are still truly appreciated.
We try to take a break and scroll through our social media accounts only to find someone else has commented about how careless or thoughtless we are. How dare we allow such horrors to happen? How could it simply continue to spread? What are we doing so wrong?
We go out in public only to find the hypocrisy of those who socially scrutinize us: employees eating on the job near customers and customers refusing to wear masks, but we still have a favorite - individuals wearing their masks tucked underneath their nose and sometimes mouth as well. There’s also some who briefly pull them underneath “because they cannot breathe.”
Exhausted, we attempt to shut out the outside world and focus on our own personal lives, but a commercial, song, or even smell reminds us of our residents. The battle is back at the forefront of our minds because it never truly leaves. We feel guilty for being away even though we work countless hours caring for them. We know we need to take care of ourselves and our day to day lives at home, but it’s no longer that simple.
And before we know it, after a struggled sleep, we wake up once more to face it all again. We’ll continue to fight until the battle is over because that’s how much we love our residents and their families.
So, remember us. Remember them. Be patient. We need continued strength and support. Know this is only a fraction of what we face.
Kendra
is an activities assistant at Piney Valley, having worked there for
five years. She recently trained and became a temporary nurse aide so
she could further assist where needed.
Monday, December 28, 2020
Woman in Nursing Home With No Family Receives Hundreds of Christmas Cards
During Christmas time, local news outlets are reporting on the goodness of humanity, from strangers flooding a lonely grandmother with Christmas cards to a couple of eight year olds deciding that what they want for Christmas is to help others in need.
Here are seven stories exemplifying the Christmas spirit – and demonstrating that the little things sometimes matter the most.
Grandma in Nursing Home Receives Hundreds of Cards
Susan Wendt, a nursing home resident in Rhode Island, felt alone this holiday season. That’s when she decided to ask for help.
“I have no close family here so it gets really lonely and can get depressing,” she told NBC 10 News. “We’ve been dealing with COVID since March, so nobody could come visit me even if they wanted to.”
Then, she asked for Christmas cards in a Facebook post.
“To be honest, I was feeling sorry for myself,” she said. “So, I thought, what if I had maybe 20 cards so I could decorate my room and make it look Christmas-y.”
The grandmother received so many cards that she’s sharing them with the other residents.
“I’m missing my grandchildren so bad and now I’m getting cards from schools, from kids all over the place,” Susan said.
“And people say there’s no love in this world,” she concluded. “They are wrong.”
Woman Donates Christmas Trees to Families in Need
Located in Florida, Kathy Jones started an effort to donate and deliver more than 100 decorated Christmas trees. One of them went to Cheryl Daly, who was unemployed last month.
While Cheryl’s tree “didn’t have an angel on top, she says it was delivered by one,” WESH 2 News reported.
Christmas is a holiday that stands out to Kathy: “Christmas for me is all about Christ,” she explained.
Eight Year Old Sells Hand ‘Santa-Tizer’ to Buy Toys for Kids in Need
This year, Flynn Bogue of Pennsylvania decided that for Christmas he wanted to help other, less fortunate children.
“I saw that I had everything that I needed and that I wanted, so I thought ‘Oh, I’ll just help kids,’” he told WNEP.
To do that, he came up with a plan, his mother, Mandy, said.
“He said ‘You know, I hear you and papa talk a lot about people who are losing their jobs because of COVID and that Christmas isn’t going to be great for everybody this year,’” she said. That’s when her son asked, “What if we created our own candy cane scented hand sanitizer and sold it so that I could buy toys for kids whose families were affected by COVID this year?”
So far, they’ve sold 500 bottles of “Santa-Tizer.”
Moms Donate 40 Stockings to NICU Moms
Three mothers in Texas – Katie, Jennifer, and Jamye – collected donations from more than 50 people for mothers of premature babies at a local hospital this Christmas. They used the funds to put together stockings full of gifts including lotion, snacks, and gift cards.
“It’s been a blessing for me, and we know exactly what it’s like because we were there years ago,” Jamye Read told KLTV 7. Katie Skinner added, “If we could just take one thing off their plate, that’s what we feel called to do.”
Eight-Year-Old Spends Savings on Those in Need
Apryl Twaddell of Colorado didn’t want presents of her own this Christmas. Instead, she told her mom, “I want to help the people who need it most for Christmas.”
“She took money from her piggy bank and we matched her,” her mother, Loretta, told KOAA News5.
The family gave away toiletries, food, blankets, and other supplies to those in need, including to a local organization that offers shelter to homeless youth.
“I feel good, because we’re doing God’s work, and that’s what matters, is love,” Apryl said.
Community Pitches in to Help Boy with Down Syndrome
Kaden Buck of Ohio has a passion for basketball. That’s why the parents of the 17-year-old with Down Syndrome looked into building a half-court in their backyard.
“I made a post on Facebook social media just saying, you know, ‘Does anybody have any recommendations for a concrete company that you trust to come out and give us a quote,’” his mother, Amanda, told Fox19 Now.
But instead of receiving quotes, companies approached them, offering to donate their services for free.
“Honestly, we were sitting out there watching them yesterday, and when it first started it was just three guys and then more and more people started showing up, and then the concrete truck pulls up and before I knew it, there’s like 15 guys,” Kaden’s mom said. “And it was overwhelming, the tears, I mean we’ve never really been on this end of generosity before.”
Woman Surprises Homeless Man with Gifts
This Christmas, Leanne Shinkle of West Virginia decided to surprise Arthur Taylor, a homeless man she knew when she previously lived in Ohio. For years, he lived under a bridge near where Leanne once worked.
“He never asked for a dime,” she said. “All he said was, ‘Please pray for me.’”
Arthur was a friendly face and even protected Leanne “numerous times when she was getting harassed walking from work to her car,” WLWT reported.
In October, she asked friends to help create a care package for him.
“It was overwhelming to see how many people just knew him in passing, how many people said, ‘I’ve been downtown and that man has helped me,’” she said of the response.
She returned to Ohio to discover Arthur had found housing through an organization that helps homeless adults battling mental illness. There, she gifted Taylor with presents including a new watch, coat, and $1,000.
In response, Arthur broke down sobbing. Among other things, he plans to share the money with other homeless individuals. Leanne called him her inspiration.
“It’s especially hard because I’ve been laid off twice in 2020,” she added, “but there’s people like Arthur in your life that always remind you that there’s things to still be thankful for.”
LifeNews Note: Katie Yoder writes for Town Hall and National Review, where this column originally appeared.

Now That Grandma Has Been Vaccinated, May I Visit Her?
A watershed moment has arrived for many families: This week health care workers from CVS and Walgreens, under contract from the federal government, will fan out to nursing homes across the country to begin vaccinating residents against the coronavirus. The shots not only will help protect the nation’s elderly and infirm — and the staff who care for them — but they raise the prospect of ending the devastating isolation many residents have felt for months.
Family members are hopeful that before too long, they will return to visiting parents and grandparents, aunts, uncles and other loved ones regularly again. We checked with experts on some common questions.
Will restrictions on visiting be lifted soon?
Probably not in a big way. Restrictions vary by state, and the federal government’s guidance on what it considers safe stands for now. They already allow visits under certain conditions. The Centers for Medicare & Medicaid Services, or C.M.S., recommended in September that outdoor visits with residents be allowed and indoor visits, too, if the facility has been free of cases for 14 days.
Some medical experts have said that those guidelines are too lax and that visits should be severely restricted, even banned. However, some of these experts are now saying that the vaccine changes the equation, somewhat.
“Once all residents are vaccinated, it opens the door for loosening of restrictions,” said Dr. Michael Wasserman, the immediate past president of the California Association of Long Term Care Medicine, a geriatrician and former executive at nursing home chains.
To allow visits, Dr. Wasserman recommends all residents of a nursing home should be vaccinated (unless they have some condition or allergy that would discourage vaccination on medical grounds); all staff members should be vaccinated; and the nursing home should have the ability to ensure that visitors test negative for the coronavirus and have been disciplined about wearing a mask in public settings.
Is the vaccine safe and effective for old and frail residents of nursing homes?
The clinical trials of the Pfizer and Moderna vaccine included people over 65, and results showed it to be safe and to work as well in older people as in younger ones.
“This vaccine has gone through testing and clinical trials to ensure it meets the highest safety standards. It also is safe to get if you already had the virus,” says a campaign to encourage people to get the shots by the American Health Care Association and National Center for Assisted Living, a combined trade group representing nursing homes and assisted-living communities.
The lead administrator for C.M.S., Seema Verma, reinforced the confidence in the shot for older patients, including those with health conditions, in a statement last week: “I urge states to prioritize nursing homes and vulnerable seniors in their distribution of the vaccine.”
The point is echoed by Dr. Sabine von Preyss-Friedman, chief medical officer of Avalon Health Care Group, which operates nursing homes, who said the new vaccines appear “safe and effective.”
If restrictions are eased, should I visit right away?
The Pfizer and Moderna vaccines both require two injections — the initial shot and a booster three or four weeks later. Dr. von Preyss-Friedman recommends waiting at least two weeks after the second shot to have a visit.
“You hope these vaccines work, but these are elderly patients,” she said. “You want to err on the side of protection.”
She said that, ideally, the visitor would also be vaccinated as well. Since shots won’t be widely available for a few months, it may be best to wait until you get your vaccine. Until then, she believes nursing homes should consider visits on a case-by-case basis.
Would visitors still need to wear a mask?
Absolutely, medical experts said. This is particularly true if they are not vaccinated, but even after they are vaccinated “until rates in the community go down,” said Dr. Joshua Uy, a geriatrician and associate professor at the University of Pennsylvania Medical School and the medical director of Renaissance Healthcare & Rehabilitation Center, a nursing home in Philadelphia.
Dr. Uy said that he hopes that the federal government would supply enough personal protective equipment so that all visitors and residents could be properly gowned for such visits.
What is being done to encourage nursing home residents to get vaccinated?
The combined nursing-home and assisted-living trade group has started a program aimed at helping nursing homes and other care facilities to explain to residents the essential need to get the vaccine. The campaign, #getvaccinated, notes: “The elderly population has a much higher risk for getting very sick, being hospitalized, or dying from Covid-19. The vaccine has been shown to provide a great deal of protection against serious illness due to Covid-19.”
But the people they love most may have more effective persuasive powers. Families can help, Dr. Uy said, by encouraging their parents and grandparents in nursing homes to get vaccinated.
“The vaccine,” he said, “is going to be our way out.”
Early Onset Alzheimer's Didn't Stop Their Love
When Jeff was in his 50s, Dawn and their son began discussing Jeff’s condition. Something didn’t seem quite right. This discussion went on for a couple years – with Dawn doing plenty of research along the way. Jeff’s mother and his grandmother had both had Alzheimer’s, but neither Dawn or their son thought it would really happen to Jeff.
They got him checked out — and Jeff was diagnosed with early-onset Alzheimer’s at age 55.
Since the diagnosis, Dawn says he acts like he did when they were first dating. “He’s just the sweetest man. It’s like we’re dating all over again. He’s just the sweetest person ever. And he tells me every day how much he loves me, and that honestly keeps me going.”
Full Article and Source:
Early-Onset Alzheimer's Didn't Stop Their Love
Sunday, December 27, 2020
New leadership promises change for Philadelphia's guardianship system
PHILADELPHIA (KYW Newsradio) — Pennsylvania's guardianship system has made headlines in recent years due to abuse after abuse of the elderly and infirm. Now the court in charge of that system in Philadelphia has a new leader.
Judge Sheila Woods-Skipper was appointed administrative judge for Philadelphia's Orphans Court last month. 70% of their workload deals with guardianships, where a third party is appointed by the court to make financial and medical decisions for a person because they lack mental capacity due to age or disability.
But the system has been rife with abuses, with stories of felons becoming guardians and stealing estates right under the noses of judges. Pennsylvania has worked to implement changes, like the Guardianship Tracking System, which allows judges to identify red flags in cases statewide.
"In that unit is a guardian investigator who looks at the reports that need to be filed but he guardian to see if there are any red flags that need to be brought to the attention of the court," explained Woods-Skipper.
Woods-Skipper set policy for the Philadelphia's Court of Common Please, and her focus has been on accessibility, for instance, using videoconferencing during the pandemic.
"I've had people come in my courtroom on gurneys, in wheelchairs because they have the right to be present, they want to be present," she said.
Elderly COVID-19 patient beaten to death by roommate at Calif. hospital, sheriff says
 |
| Click to Watch Video |
LANCASTER, Calif. (AP) - An elderly man hospitalized in Southern California for treatment of COVID-19 was fatally struck by a roommate who became annoyed when the victim began praying, the Los Angeles County Sheriff’s Department said Wednesday.
The 82-year-old victim was struck with an oxygen tank on Dec. 17 while housed in a two-person room at Antelope Valley Hospital in Lancaster and died the next day, the department said in a statement. His name was not released.
The suspect, Jesse Martinez, 37, was arrested and charged with murder and other crimes, the department said.
Martinez was being held on $1 million bail and was scheduled for an initial court appearance on Dec. 28. It was not immediately known if he has a lawyer who could speak on his behalf.
The Sheriff’s Department said the investigation was continuing.
Reassuring Note to Dementia Patient
by Elizabeth NelsonMost people think dementia is merely a simple loss of memory, but it can be so much more than that. Memories don’t always just get lost; sometimes they get distorted, or new memories get made up in the person’s head. The confusion of so many memories, both real and fake, can cause severe anxiety and other serious issues. Awareness of this common problem is important to make sure that all people with dementia are cared for as well as possible, including their psychological needs.
Recently, a Reddit user posted a photo of a special note a woman wrote to her mother with dementia. The message, written in different colors on a whiteboard, serve as a constant reminder to her elderly mother that the things she’s anxious about are not real concerns. The reminders serve to calm her down when she believes there’s a problem.
The message reads:
“Your meals are paid for.
You’re okay.
Everyone’s fine.
You are not moving.
No one else is moving.
Keep drinking; it will help your memory.
You don’t owe anyone any money.
You haven’t upset anyone.”
But what’s truly amazing about this message is that it has stricken a chord with so many other caregivers and family members of someone with dementia who has very similar anxieties. The post has 111k upvotes and 2.2k comments. It seems that many people have witnessed a loved one with this horrible disease suffer from crippling fears of not being able to pay for things or thinking other people are mad at them.
“‘You can use the bathroom whenever you like,'” wrote Reddit user Kryptosis. “My ex’s great grandma used to think she had been told she wasn’t allowed to go to the bathroom 🙁 Sad and very dangerous.”
Source:
The Alzheimer's Site
Saturday, December 26, 2020
Owner of Texas Chain of Hospice Companies Sentenced for $150 Million Health Care Fraud and Money Laundering Scheme
A corporate executive has been ordered to serve 20 years in prison after his conviction related to falsely telling thousands of patients with long-term incurable diseases, such as Alzheimers and dementia, they had less than six months to live and subsequently enrolling them in hospice programs.
A federal jury in McAllen, Texas, convicted Rodney Mesquias, 48, of San Antonio, Texas. The one-month trial in November 2019 was one of the first criminal hospice fraud prosecutions the Department of Justice has presented to a federal jury.
Today, U.S. District Court Judge Rolanda Olvera ordered Mesquias to serve a total of 240 months in federal prison and to pay $120 million in restitution.
“Mesquias funded his lavish lifestyle by exploiting patients with long-term, incurable diseases by enrolling them in expensive but unnecessary hospice services,” said Acting Assistant Attorney General Brian C. Rabbitt of the Justice Department’s Criminal Division. “This significant sentence represents the department’s continued commitment to pursue those who orchestrate and commit healthcare fraud schemes.”
“Financial healthcare fraud is abhorrent enough, but to fraudulently diagnose patients with dementia or Alzheimer’s is the pinnacle of medical cruelness to both the patient and their family,” said U.S. Attorney Ryan K. Patrick of the Southern District of Texas. “They falsely gave patients life ending diagnosis and they will pay the price with years behinds bars.”
“Families seek to give comfort and support to their ailing loved ones when all other medical options are gone,” said Special Agent in Charge Christopher Combs of the FBI’s San Antonio Division. “It is unconscionable and evil to prey upon the most vulnerable in our community to commit fraud against government-funded programs. The FBI is committed to protecting our communities from those who may not have the strength to protect themselves.”
“Mesquias’ scheme included paying kickbacks to physicians and fraudulently enrolling vulnerable beneficiaries in hospice care that prevented them from accessing curative care – all done to steal millions of dollars from Medicare to fund lavish personal spending,” said Special Agent in Charge Miranda L. Bennett of the U.S. Department of Health and Human Services Office of Inspector General’s (HHS-OIG) Dallas Region. “This victimization is intolerable, and our investigators and law enforcement partners will continue to work hard to bring such criminals to justice and to protect those relying on federal health care programs.”
Mesquias and his co-conspirator Henry McInnis, 48, were both convicted of one count each of conspiracy to commit health care fraud, conspiracy to commit money laundering and conspiracy to obstruct justice as well as six counts of health care fraud. Mesquias was separately convicted on one count of conspiracy to pay and receive kickbacks.
From 2009 to 2018, Mesquias orchestrated a scheme that involved $150 million in false and fraudulent claims for hospice and other health care services. Mesquias owned and controlled the Merida Group, a large health care company that operated dozens of locations throughout Texas.
According to evidence presented at trial, Mesquias and the Merida Group adopted a strategy to market their hospice programs as providing medical benefits “you don’t have to die to use.” They also aggressively enrolled patients with long-term incurable diseases, such as Alzheimers and dementia, and limited mental capacity who lived at group homes, nursing homes and in housing projects.
In some instances, Merida Group marketers falsely told patients they had less than six months to live and sent chaplains to lie to the patients. They also discussed last rites and preparation for their imminent death.
Hospice services require patients to be suffering from a terminal illness expected to result in death within six months. Not only were patients not in such circumstances, they were walking, driving, working and even coaching athletic sporting events in some instances. However, Mesquias and others kept patients on services for multiple years in order to increase revenue.
Placing patients on such palliative hospice care meant they were unable to obtain medical coverage for curative medical services.
Mesquias also fired employees who refused to go along with the fraud. He often directed them not to “[expletive] with his patients or [expletive] with his money” by discharging patients from services. One co-conspirator said with respect to hospice patients “the way you make money is by keeping them alive as long as possible.” This included engaging in surgical and other medical interventions that were designed to extend life through the use of medical technologies, according to trial testimony.
The evidence further established Mesquias obstructed justice by causing the creation of false and fictitious medical records. Further, Mesquias produced them to a federal grand jury in order to attempt to avoid indictment. The records added false diagnostic information, making it appear that patients were dying when, in fact, they were not.
Mesquias also was convicted in connection with laundering the proceeds of the fraud. The jury found they used monies to purchase expensive vehicles such as a Porsche, expensive jewelry, luxury clothing from high-end retailers such as Louis Vuitton, exclusive real estate, season tickets for premium sporting events and a security detail and bottle service at high-end Las Vegas nightclubs. Mesquias also treated physicians to lavish parties at these elite nightclubs, providing them with tens of thousands of dollars in alcohol and other perks in exchange for medically unnecessary patient referrals.
McInnis will be sentenced at a later date. Two other co-conspirators have pleaded guilty and are awaiting sentencing.
The Department of Health and Human Service – Office of Inspector General (DHHS-OIG); FBI and Texas Health and Human Services Commission conducted the investigation. Assistant Chief Jacob Foster and Trial Attorney Kevin Lowell of the Criminal Division’s Fraud Section and Assistant U.S. Attorney Andrew Swartz of the Southern District of Texas are prosecuting the case.
The Fraud Section leads the Health Care Fraud Strike Force. Since its inception in March 2007, the Health Care Fraud Strike Force, which maintains 15 strike forces operating in 24 districts, has charged more than 4,200 defendants who have collectively billed the Medicare program for nearly $19 billion. In addition, DHHS Centers for Medicare & Medicaid Services, working in conjunction with the DHHS-OIG, are taking steps to increase accountability and decrease the presence of fraudulent providers.
The year 2020 marks the 150th anniversary of the Department of Justice. Learn more about the history of our agency at www.Justice.gov/Celebrating150Years.
Attorney arrested for fraudulently billing insurers $300,000
The attorney, 73-year-old Moses Luna, allegedly defrauded insurers to collect $311,220 in workers’ compensation fees. A joint investigation by the California Department of Insurance and the Orange County District Attorney’s Office found that Luna created a company called Adelante Interpreting, through which he fraudulently billed 20 separate insurance carriers for translation and interpreting services.
According to investigators, Luna exclusively referred his own workers’ compensation clients to Adelante Interpreting to fraudulently collect fees from insurers. The fees the attorney received were for translation and interpreting services rendered to workers’ compensation claimants during depositions and medical appointments.
An official release from the California Department of Insurance said that Luna failed to disclose his financial interest in Adelante Interpreting, as required by law. He allegedly used his daughter’s name for the paperwork, but Luna ultimately controlled all aspects of the interpreting and translation company – including administrative protocols, employee protocols, independent contractor protocols, as well as billing and collection protocols.
The state Department of Insurance also disclosed that the insurance companies affected by Luna’s scheme include ACM, AIG, Amtrust, BHHC, CompWest, Employers, ESIS, Farmers, Hartford, ICW, Liberty Mutual, Markel, Matrix, Midwest, Sedgwick, SCIF, Sentry, Travelers, York and Zurich.
Luna is set to return to court next year, on January 19, 2021. The
case is being prosecuted by the Orange County District Attorney’s
Office.
Grant Provides New Assistance for Elderly, Disabled Adult Abuse Victims
Alabama Gov. Kay Ivey has awarded $1.9 million to aid disabled adults and elderly persons who are victims of abuse.
The Department of Human Resources will use the grant to provide in-home or temporary placement support for victims who are put through acts of abuse, neglect and exploitation. This financial assistance will help create a safe environment for the elderly and disabled adult victims by providing in-home care, enabling them to remain in their homes once the perpetrators have been removed. Further, the funds will also be used in relocating victims to assisted living facilities or nursing homes.
Each measure is temporary until more stable options are discovered.
“No one should ever be subject to abuse of any kind, and it is reprehensible that it should happen to someone who may not have the physical or mental capabilities to resist or be aware of those acts,” Gov. Ivey said. “This grant will assure elderly and disabled adults who are victims of physical and mental abuse are taken out of harm’s way and receive needed care.”
The Alabama Department of Economic and Community Affairs administered the grant through funds made available by the United States Department of Justice. ADECA operates an array of programs meant to support law enforcement, water resource management, victims, recreation, economic development and energy conservation.
“ADECA is pleased to join with Gov. Ivey and the Alabama Department of Human Resources to provide solutions for these victims,” said ADECA Director Kenneth Boswell on the grant.
To report any abuse, neglect or exploitation of elderly or disabled victims, please contact the Department of Human Recourses’ Adult Protective Services Division at 334-242-1350.
Friday, December 25, 2020
Edith + Eddie: America's Oldest Interracial Couple
On this Christmas day, we thought it fitting to remind everyone of the wonderful documentary, "Edith + Eddie." This heartfelt film by filmmaker Laura Checkoway was a front runner for an Oscar in 2018 and when you watch it, you'll see why.
The story begins with Edith and Eddie's deep love for each other. And although their love never died, their lives changed forever when guardianship interfered with their devotion and their final days together.
Source:
YouTube: Edith + Eddie
In the Bleak Midwinter - (Camille and Her Mother) Merry Christmas!
Enjoy the joyful sounds of hope, love, family, peace and Christmas - a gift directly from the hearts of Camille and her Mom to NASGA members and supporters and their families.
Merry Christmas!
Source:
In the Bleak Midwinter - Single
Thursday, December 24, 2020
Married 65 Years; Their Love Endures Despite Dementia

Unfortunately, Ruby began showing signs of dementia ten years ago, and her memory has declined. She often forgets the identity of those close to her, but she has never forgotten her husband.
“Wonderful, I just can’t find anything wrong with him yet, and you see how long we’ve been married?” Ruby says of Harold. “You suppose I’ll find anything? I don’t know at this point!”
Full Article and Source:
Married 65 Years; Their Love Endures Despite Dementia
Ohio Assisted Living Builds "Hugging Wall" for Residents
Full Article, Video and Source:
Richland County Assisted Living Builds Hugging Door for Residents
















