 |
By Suzy Khimm
The moment that Tammy Roberg stepped off the elevator, she could hear her father’s booming voice.
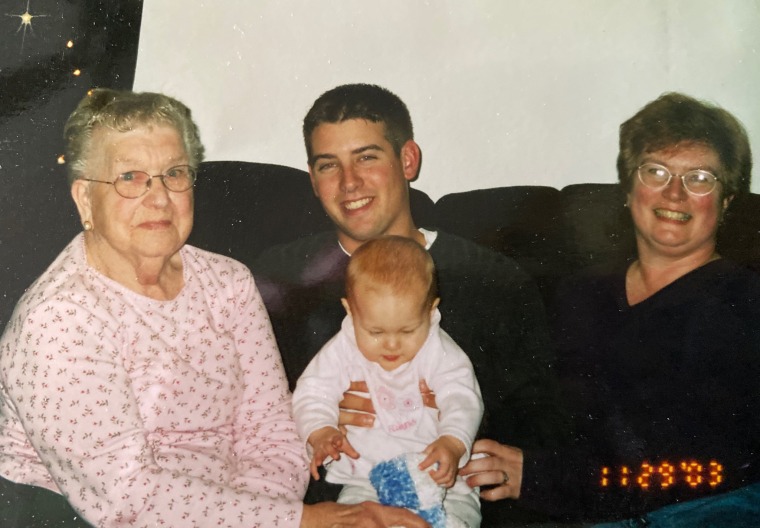
Chester Peske, 98, loved to sit in the lunchroom at Copperfield Hill and talk to the other memory care residents about everything from the weather to the history of the highway that connected his hometown to downtown Minneapolis, 6 miles away. While he had Alzheimer’s disease, Peske still recognized his children when they came to the Robbinsdale, Minnesota, facility for weekly visits.
“He would talk and talk and talk,” Roberg said with a laugh.
Then, in March, there was almost no one that Peske could talk to.
When the pandemic hit, long-term care facilities across the country, including Copperfield Hill, shut their doors to visitors and largely kept residents to their rooms, suspending most group activities and communal meals to protect residents from Covid-19. Peske was hard of hearing, so phone calls were a struggle. Roberg’s only lifeline to her father was the staff of the facility, who reassured her that he was doing well.
 |
| Click to Watch Video |
The first sign of a problem came in mid-May when her father tested positive for Covid-19. Roberg prayed for his health, but was relieved when his case appeared to be asymptomatic.
Then in late May, Roberg got another alarming call from the facility. It wasn’t the virus, they said — something else was wrong. “His head was down into his chest, and he was sitting slumped in his wheelchair,” her father’s aide said, according to Roberg. “He was not his perky, chatty self.”
Roberg later learned that her father, who’d always had a healthy appetite, had been losing weight. Even more isolated in quarantine after his Covid-19 diagnosis, he was becoming quiet and disengaged, even with the staff members who tended to him, a nurse later told her.
He still had no coronavirus symptoms — he was just withdrawn, according to Roberg and an administrator at Copperfield Hill. Roberg was hopeful that he would bounce back with more hands-on attention from the facility. But four days later, on June 2, she got another call: She should come right away. Her father was dying.
That morning, Roberg flew in from Wisconsin and met her brother in the parking lot of Copperfield Hill. Together they walked into the entryway of the facility, where they were temperature-checked, and then put on gowns, gloves and face shields. A nurse finally brought them up to her father’s floor and opened the door.
“Oh wait a minute—” she said, stopping short. “I think he’s gone.”
Roberg gasped when she saw her father’s gaunt body lying on the bed. After three months of separation, she missed her only chance to see her father by minutes.
His death certificate listed the cause of death as the progression of Alzheimer’s disease and “social isolation / failure to thrive related to COVID-19 restrictions.”
Social isolation was listed as a contributing cause of death for at least nine other Minnesotans — almost all long-term care residents — from June to September, according to state death records; no deaths in the previous two years cited social isolation as a cause.
One of the nurses who treated Peske later described his deterioration as a burning candle with no oxygen left to draw from the air. It was as if a light had gone out, Roberg said: “He couldn’t survive from being isolated.”

The unseen cost of lockdowns
The effort to shield elderly, frail and disabled residents from the coronavirus has created another wrenching health crisis: The confinement meant to protect the most vulnerable is also threatening their lives.
“The isolation is robbing them of whatever good days they have left — it accelerates the aging process,” Joshua Uy, associate professor at the University of Pennsylvania Perelman School of Medicine, said.
“You see increased falls, decrease in strength and ability to ambulate. You see an acceleration of dementia, because there is no rhythm to your day. There isn’t a single part of a person’s life that isn’t affected.”

While there is no comprehensive tally of elderly people dying from causes linked to social isolation and confinement, evidence is mounting that restrictions related to Covid-19 are taking a toll on their health, according to a review of recent research and interviews with medical experts and dozens of families across the country. The phenomenon is far harder to track than the number of Covid-19 deaths linked to long-term care facilities — 84,000 as of early October, according to the Kaiser Family Foundation — as it is unusual to list isolation as an official cause of death. But the harms are still real, experts say.
One recent study of a Chicago-area nursing home found that from December 2019 to the end of April 2020, two-thirds of the residents had lost weight, in some cases dramatically — a change that researchers attributed to reduced social interaction, the cessation of family visits and schedule changes due to the pandemic.
Confinement, social isolation and the lack of external stimulation are also fueling cognitive decline and depression, which in turn increase the risk of high blood pressure, heart disease and stroke, according to Dr. Louise Aronson, a geriatrician and professor of medicine at the University of California, San Francisco.
“Sometimes the doors to their rooms are open, and you just see someone sitting in a chair with tears running down their face,” Aronson, who is assisting San Francisco’s response to the pandemic in long-term care facilities, said. “People ask me, ‘Is this the rest of my life? If so, I don’t want to go on.’”
Do you have a story to share about how the coronavirus is affecting nursing homes? Contact us
While most states have begun allowing some form of routine in-person visits for long-term care facilities, the guidelines vary widely, and many restrictions remain — not only to protect residents, but also vulnerable front-line staff members, many of whom are low-wage Black and Hispanic workers. Some states and facilities are only allowing limited indoor visits, and colder weather is already curtailing outdoor visits. Many nursing homes have resumed communal dining and group activities, but still require residents to remain distanced from one another. And a single case of the virus can put a facility back on lockdown for weeks.
The threat from the pandemic has not receded: On Friday, the U.S. hit a new record number of Covid-19 cases, and nursing homes from Massachusetts to Wisconsin are reporting new outbreaks. At the same time, policymakers need to weigh the competing risks, said David Grabowski, a health policy professor at Harvard Medical School, who recently served on an independent federal commission that recommended expanding in-person visitation at long-term care facilities.
“We’ve locked these older adults in their rooms in the name of safety without thinking about the unintended consequences here,” Grabowski said. “In many respects, the side effects are worse than the potential harm of a slightly higher risk of infection.”

Strict, prolonged lockdowns can dramatically alter residents’ health. Uy said that he saw some patients rapidly lose the ability to perform basic tasks — such as standing, feeding themselves and swallowing safely — while confined to their rooms. Physical therapy and other rehabilitation services have also been cut back because of the pandemic.
“Until the pandemic, ‘sudden frailty’ would have been an oxymoron,” Aronson said. “Normally, it would take months to years, and we are now seeing it in weeks.”
But while deadly coronavirus outbreaks at nursing homes tend to grab headlines, the slower-moving health crisis inside these facilities caused by social isolation and confinement remains largely invisible.
Unlike cases of Covid-19, it is not always clear when a resident’s health is deteriorating because of pandemic-related restrictions, given the complex medical issues that brought them to the facilities in the first place. “Failure to thrive,” for instance, is often characterized by weight loss, reduced appetite and lower activity levels — symptoms that could also be linked to other underlying health conditions. But the biggest marker is psychological, and closely linked to isolation.
“It means, they give up,” said Dr. Joseph Ouslander, a professor at Florida Atlantic University’s Charles Schmidt College of Medicine. “You do everything to get them to participate, to get them to eat, and despite that they continue to go downhill.”
‘I would do anything to get away’
Beverly Noody used to drop by her mother’s assisted living facility in upstate New York at least twice a week. The first thing she would do: Walk over to her mother’s chair to see that her feet were propped up.
Barbara White, 94, had congestive heart failure, so her limbs tended to swell from fluid buildup. She was supposed to keep her legs elevated when she was sitting down, and to get up and about a few times a day. But her daughter knew that wouldn’t always happen unless she made sure it did. “She never had her feet up when I came to visit,” Noody said. “If her ankles and knees were swollen, I would have noticed it.”
Two months into the pandemic, Noody got a call that her mother was en route to the hospital because of dangerous swelling in her legs. She recovered, but the same thing happened again in June, Noody said. She could no longer use her walker to get around safely, as she kept falling. Her condition ultimately deteriorated so much that she was moved out of assisted living and into the adjoining nursing home, Premier Genesee, where she could be supervised around the clock.
Noody had always thought of her mother as the no-nonsense type, true to her German roots. But in July, when she was helping to move her mother’s possessions into the nursing home, she found a letter that White had written during the pandemic, but hadn’t given her.
"Beverly, I want to come home for good. I don’t know how to get out of here,” her mother wrote. “I would do anything to get away. I was told today this was forever. Do you know how I can get away?”
New York was the first state to ban visitors from nursing homes in mid-March, and other states quickly followed suit. The virus has still taken a devastating toll on residents, many of whom were highly vulnerable because of their advanced age and underlying health conditions. At least 6,600 long-term care residents in New York have died from Covid-19, an undercount that doesn’t include those who died after they were taken to the hospital.
While nursing home cases and deaths have ebbed since the spring, New York has remained cautious about reopening long-term care facilities to visitors. In July, the state announced that limited outdoor visits and residential activities could resume, but only after facilities were free of Covid-19 cases for 28 days.
Full coverage of the coronavirus outbreak
Premier Genesee was preparing to begin outdoor visits under the state’s new guidelines when a staff member tested positive in late July, pushing back the reopening, as required by the state. Noody and other angry family members held a local rally in early September protesting the state’s visitation restrictions; other grassroots groups have held similar protests elsewhere in New York and other states.
“If she got Covid and she passed away, I would be heartbroken,” Noody said of her mother. “But do I want her to live walled up in a room? Absolutely not. It’s not fair. Nobody wants to live like that, but they're not even given a choice.”
Under mounting pressure, New York officials relented in mid-September and lowered the threshold for in-person visits to 14 days without a coronavirus case. They also added a requirement for visitors to have a verified negative Covid-19 test. There are still strict caps on the number of visitors allowed in the facility, as well as social distancing and mask requirements.
New York officials say the restrictions are critical to protecting residents and front-line workers at these facilities. “This pandemic is not over,” Jill Montag, a spokeswoman for the state health department, said in a statement. “Our decisions will continue to be driven by data and science, and now is not the time for anybody to let their guard down.”

Diminishing quality of life
The Covid-19 restrictions are especially painful when residents themselves can’t understand why their family members have stopped coming to visit. More than half of nursing home residents have moderate or severe cognitive impairment from Alzheimer’s, dementia and other conditions, according to the Centers for Medicare and Medicaid Services.
Before the pandemic, Adele Billig constantly circulated throughout her nursing home in Delray Beach, Florida, always showing up for bingo, poker night and karaoke, where she loved belting Frank Sinatra. “I’m never in my room, so don’t call my room, because you’re not going to get me,” the 95-year-old often told her daughter, Melinda.
Under lockdown, Adele’s social life disappeared. Mostly confined to her room, she had little to keep her engaged: She had trouble following television programs, and phone calls could be difficult, as her hearing aids regularly went missing. “She’d say, ‘I can’t hear you, I can’t hear you.’ Then she’d just give up,” Melinda said. Sometimes when Melinda called, her mother assumed that her daughter was in the building, waiting to come up for a visit, and was crestfallen when she learned she wasn’t there.
Adele began sleeping more and more, even falling asleep during their phone calls, which had never happened before, Melinda said. By June, she was developing wounds that were not healing — a serious sign that her body was breaking down. But the most upsetting part for Melinda was the feeling that her mother didn’t fully grasp why she had stopped visiting, as her memory was spotty.
“I wish I could be there with you,” Melinda told her mother in July.
“If you say so,” her mother responded flatly.
It was the last conversation they had. The next week, the nursing home called to tell Melinda that her mother had died. The official cause of death was heart failure, but Melinda doesn’t think that conveys the full story.
“Part of why she died,” she said, “is that her quality of life had diminished to such a point that there wasn’t any.”
‘Why can’t I hold her hand?’
Even when family visits resume, there are usually significant restrictions in place. When Gelsey Randazzo Markese went to see her grandmother Rose Violet Randazzo for the first time in seven months, the rules made her almost regret showing up at all.
It was the last week of September when she arrived at the Edna Tina Wilson Living Center in Rochester, New York, with her grandfather Vincent Randazzo, who had been married to her grandmother for 69 years. Markese had been raised by her grandparents, who adopted her as a baby, so it was especially hard to be separated from Rose Violet for so long.

When a staff member brought her out in a wheelchair, Rose Violet, 91, instinctively stretched out both arms to touch Markese, then broke down sobbing when the aide told her that they had to remain at least 6 feet apart.
“My baby, my baby...” she wept, her arms still reaching for her granddaughter, who was also in tears. “She’s my baby.”
It was a wrenching experience for Markese, who was seven months pregnant and had been waiting to tell her grandmother in person. “To me it was almost more tortuous being there, so close but not being able to touch,” she said. “It was like being punched in the stomach.”
Markese and other family members are now pushing New York officials to create a program that would enable them to be recognized as “essential caregivers” — a designation that would allow them to provide hands-on assistance and companionship for loved ones in long-term care facilities.
In June, Indiana became the first state to permit essential caregiver visits for family members who had tended to residents at least two times a week prior to the pandemic, subjecting them to the same Covid-19 testing requirements as staff members. Minnesota, New Jersey, Florida, Texas and other states have made similar accommodations for family members, stressing their role in monitoring their loved ones and advocating on their behalf. Florida recently announced that facilities can allow outdoor visits even if they have recently reported coronavirus cases.
Markese knows how deadly Covid-19 can be; 11 residents and one staff member have died of the virus at her grandmother’s nursing home, according to federal data. But she believes that visits without social distancing can be done safely.
“If we follow the same protocols in place as the staff members do — the staff members who bathe my grandmother and help toilet her and help comfort her by holding her hand — then why can't I hold her hand? Why can't I give her a hug?” Markese said. “Why can't my grandfather embrace her when she's crying out to touch him?”

To address the impact of prolonged isolation, the Centers for Medicare and Medicaid Services issued new guidance in September to help expand “compassion care” visits in nursing homes. In addition to allowing end-of-life visits, facilities could also permit families to visit residents who are losing weight or dehydrated and need encouragement to eat or drink, as well as residents who are “experiencing emotional distress, seldom speaking, or crying more frequently,” the new guidance said.
State and local governments, however, can still impose stricter rules for nursing home visits and usually give facilities considerable leeway in deciding when to reopen. The push for more visitation is also coming amid signs that the pandemic could reach a dangerous new crisis point in the fall and winter, increasing the risk of community spread.
Nearly eight months into the pandemic, some long-term care facilities are still struggling to protect themselves from Covid-19. Nursing homes across the country continue to report a lack of reliable testing and personal protective equipment, as well as staffing shortages. Without adequate protections in place, in-person visits could put both residents and staff members at greater risk.
Industry lobbyists are now pushing Congress for more money for facilities to prepare for the next wave of the virus, while admitting there is a tough trade-off when it comes to protecting residents.
“We too are concerned about prolonged social isolation for our residents,” the American Health Care Association, which represents for-profit long-term care facilities, said in a statement. “With cases rising in many parts of the country, we must be vigilant about protecting our nation’s most vulnerable, but balance that with the need to stay connected with loved ones.”
‘It didn’t have to happen’
Tammy Roberg is still haunted by the circumstances of her father’s death. Shocked by the weight he had lost at the end, she asked the staff to show the logs of what he ate at every meal, only to be told there weren’t any. A nurse later told Roberg that isolation often prompts deep depression among Alzheimer’s patients, which helped explain why her father had deteriorated so quickly.
Ashley Fjelstad, a spokeswoman for Copperfield Hill, said that Peske’s health had not declined dramatically until his final days. She said the facility typically only notes if residents refuse to eat at all, not the portions they eat at each meal. And she noted that changes in routine are especially disruptive for those with Alzheimer’s disease: The common areas of the facility, where residents can socialize and do activities together, “are the heart and soul of memory care,” she said.
On the morning of her father’s death, Roberg sat down beside his body and took his hand in her own. She prayed and told her father that she loved him. But she couldn’t shake how he looked lying there. “Why was he so skinny?” she wondered. “When did he last eat?”
Several weeks after his death, Minnesota enacted a policy allowing essential family caregiver visits in long-term care facilities, including Copperfield Hill.
Roberg never got that time. Months later, she keeps holding onto the same thought: “It didn’t have to happen.”

No comments:
Post a Comment